
Taken as a whole, athletes participating in sport that present with signs and symptoms suggestive of EDS or other hypermobile syndromes, should have a comprehensive evaluation including joint mobility, muscular strength, balance and coordination, in addition to systemic issues including gastrointestinal, cardiology, psychiatry and neurology. The relative muscular weakness of athletes presenting with EDS and hypermobile syndromes may require additional time or effort to improve strength to be able to perform well and reduce injury risk. The good news is that strength training has a protective effect on joints, improves pain experience and reduces the risk of fall-related injuries. It is imperative that the athlete and their trainers keep an eye on fatigue levels, as individuals with EDS tend to fatigue earlier compared to their non-EDS peers. If athletes with EDS are managing an injury, it is usually best to continue activity with modifications, rather than completely stop.
While EDS and hypermobile syndromes are highly prevalent in the performing arts community, awareness of the associated complications and injury-risk factors is not fully understood with all health care providers. Seeking physical therapy treatment from a therapist that understands the physical and emotional demands of performing arts in addition to complications with EDS can make an enormous difference in an athletes career.
If you are an athlete experiencing EDS or hypermobility, and are concerned about returning to sport, give our office a call. Dr. Abbate has years of experience helping hundreds of professional performing artists at Royal Caribbean and Celebrity Cruises. If he can help them, he can help you!
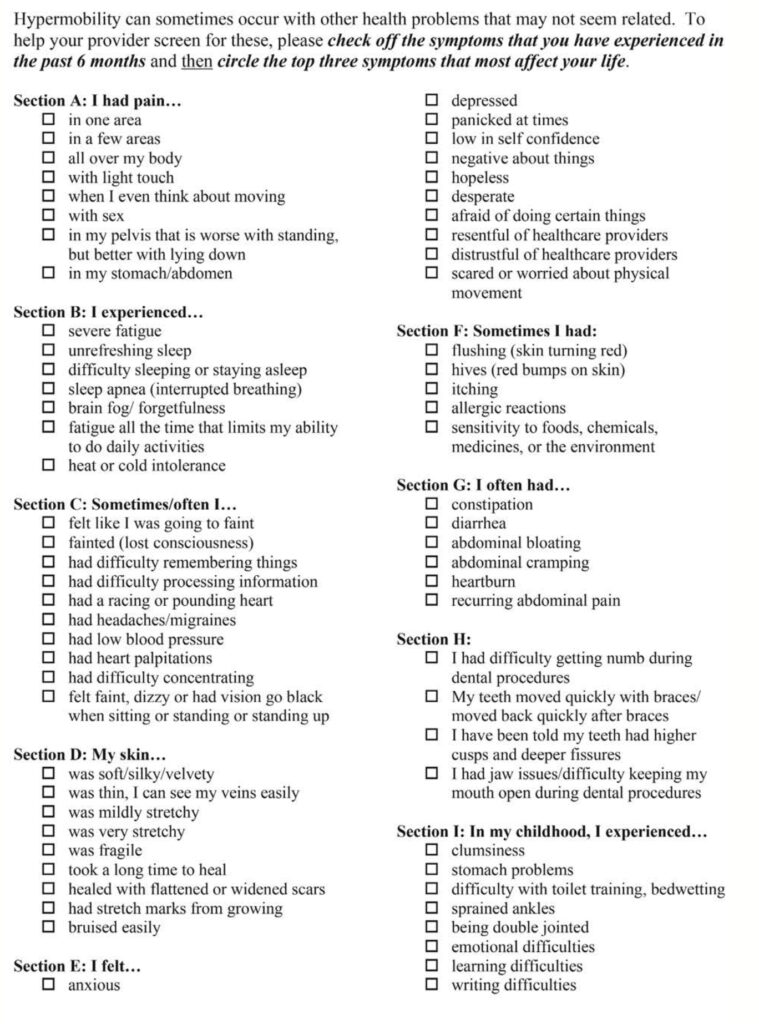
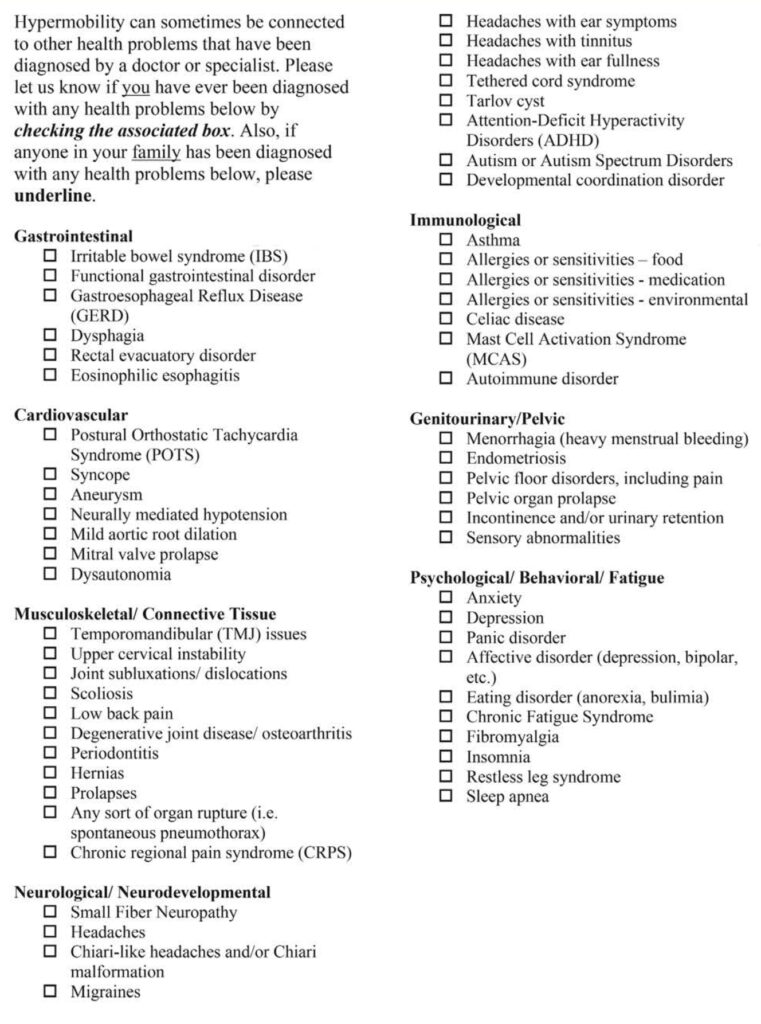
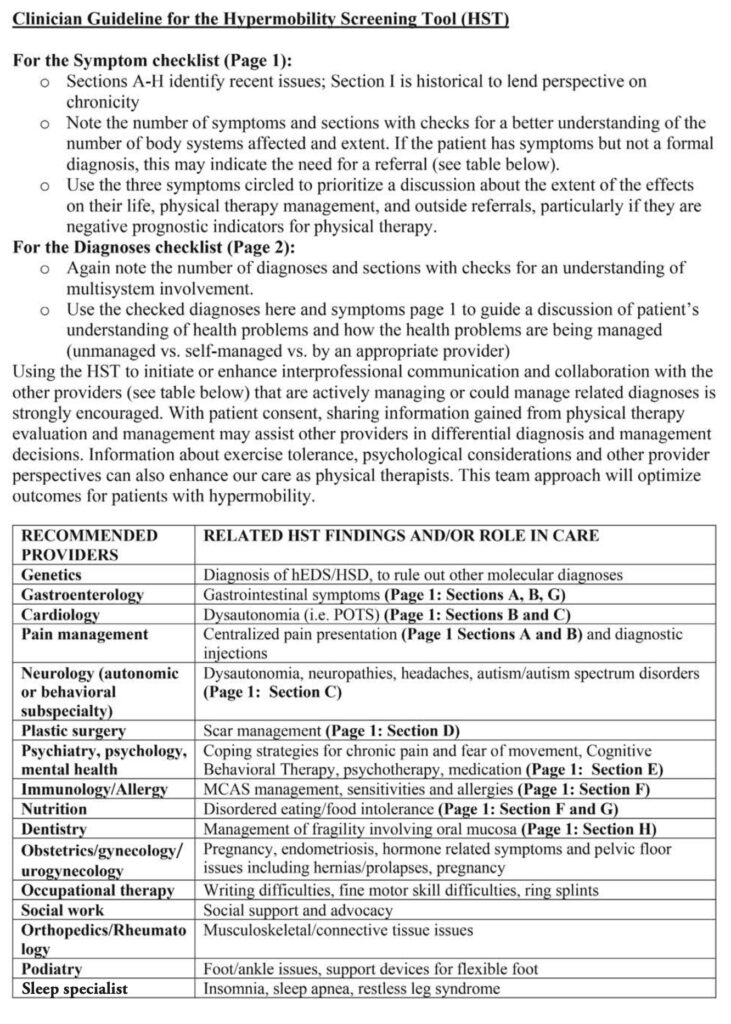
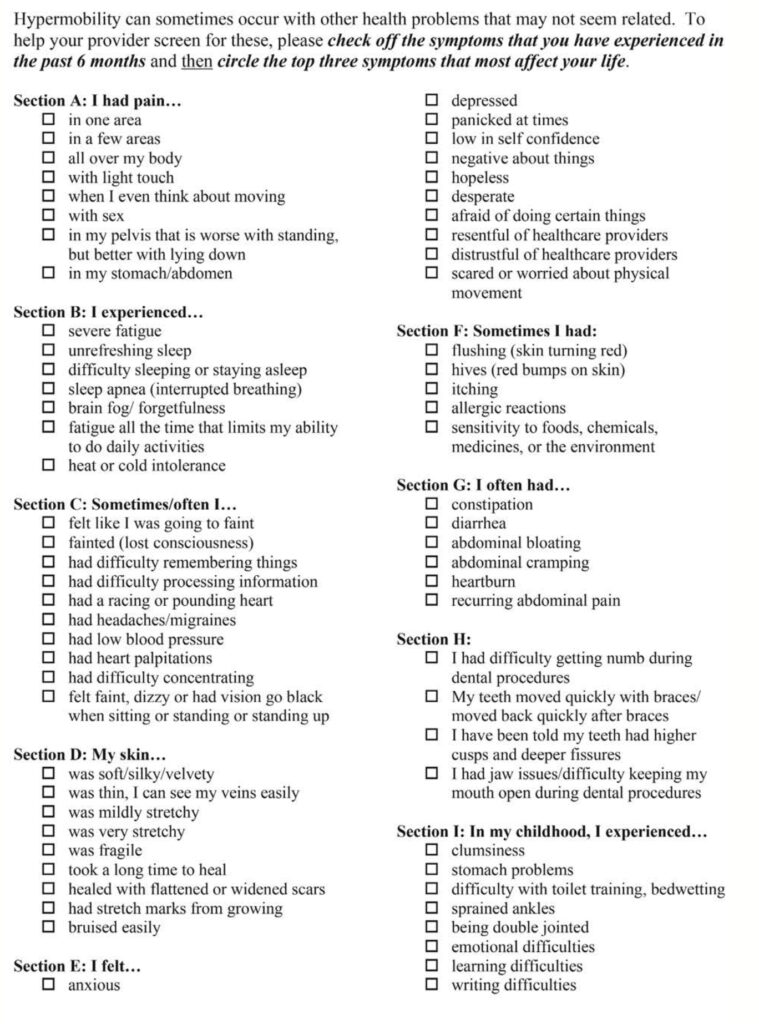
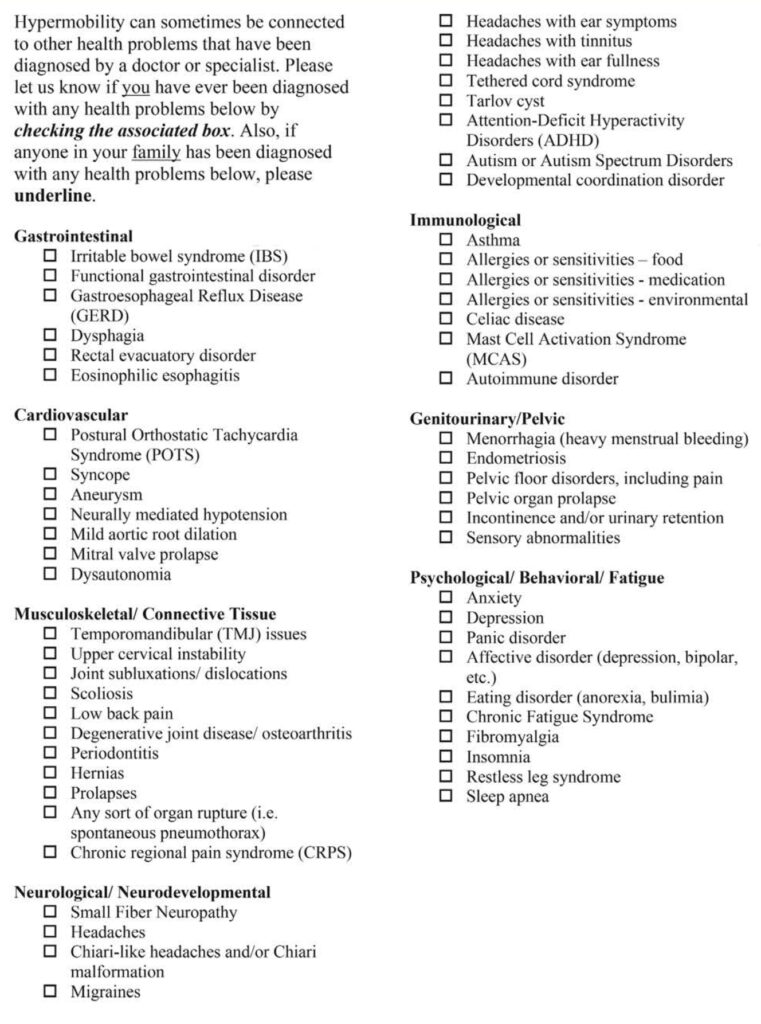
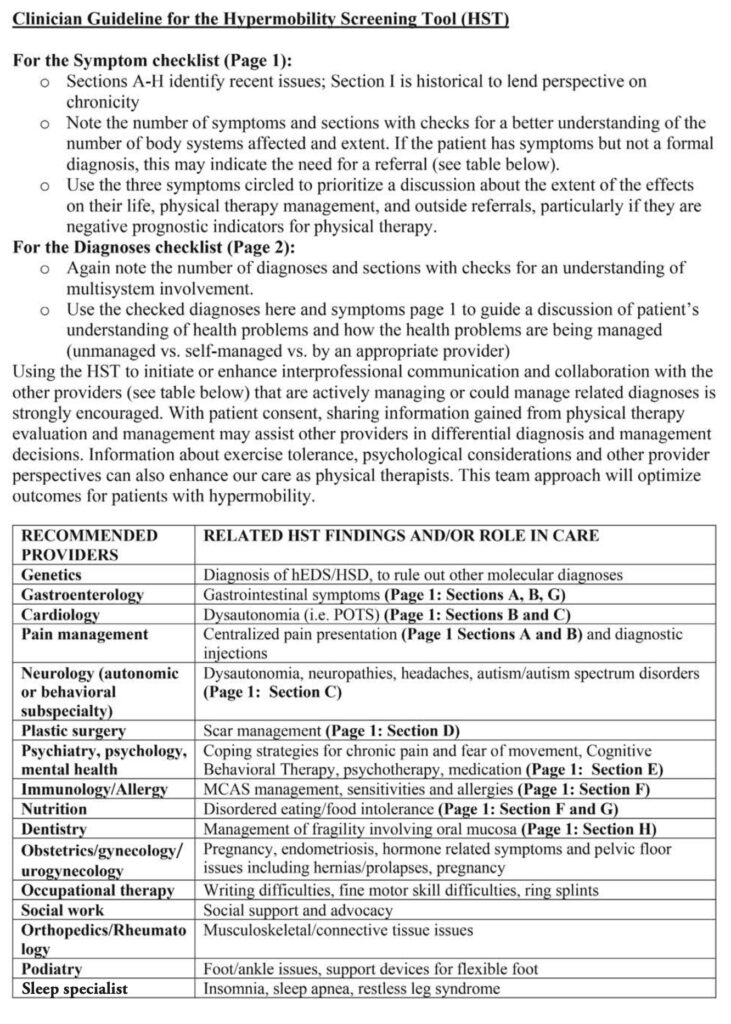
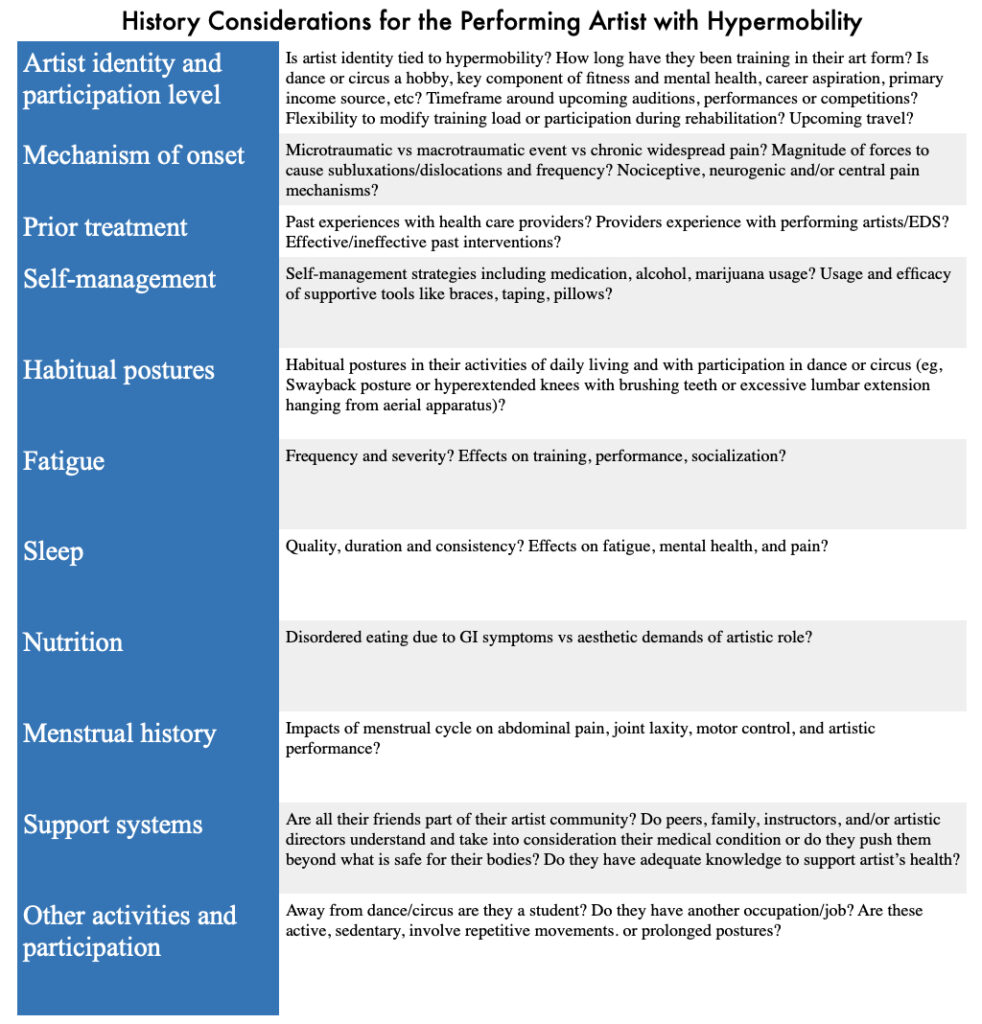
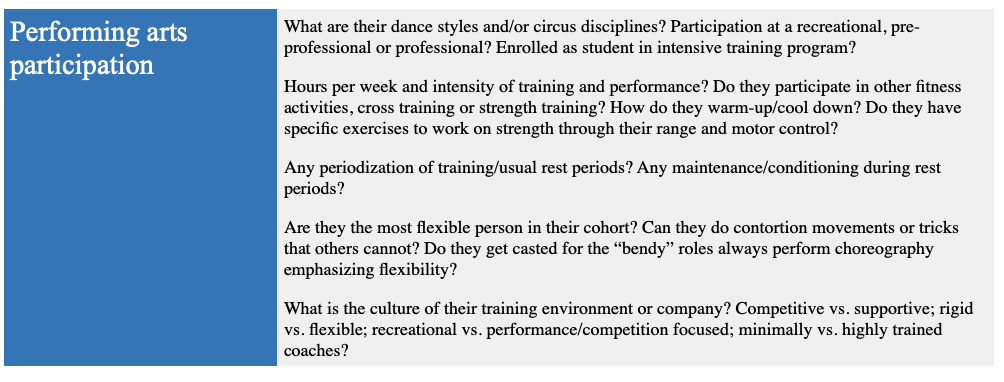
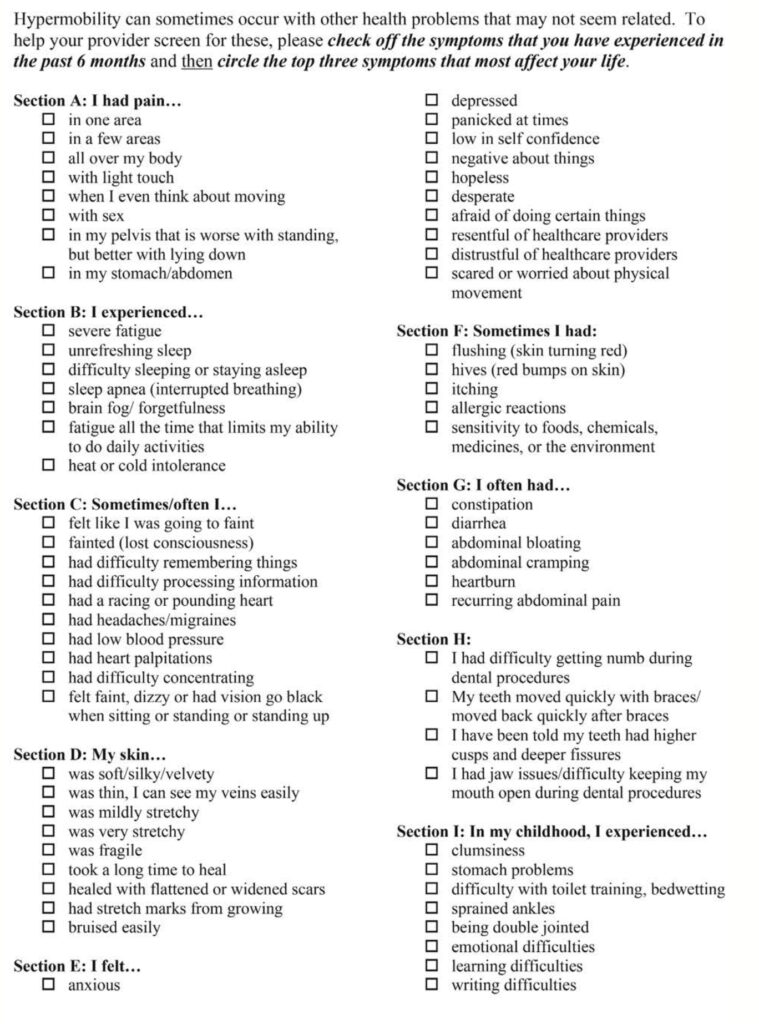
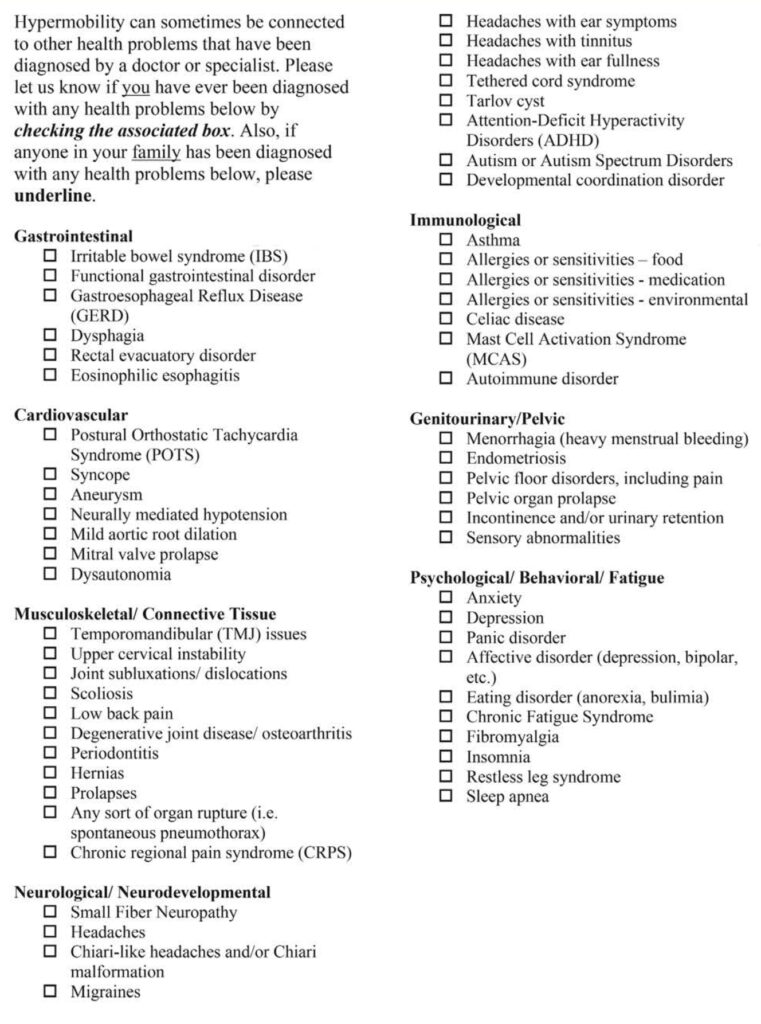
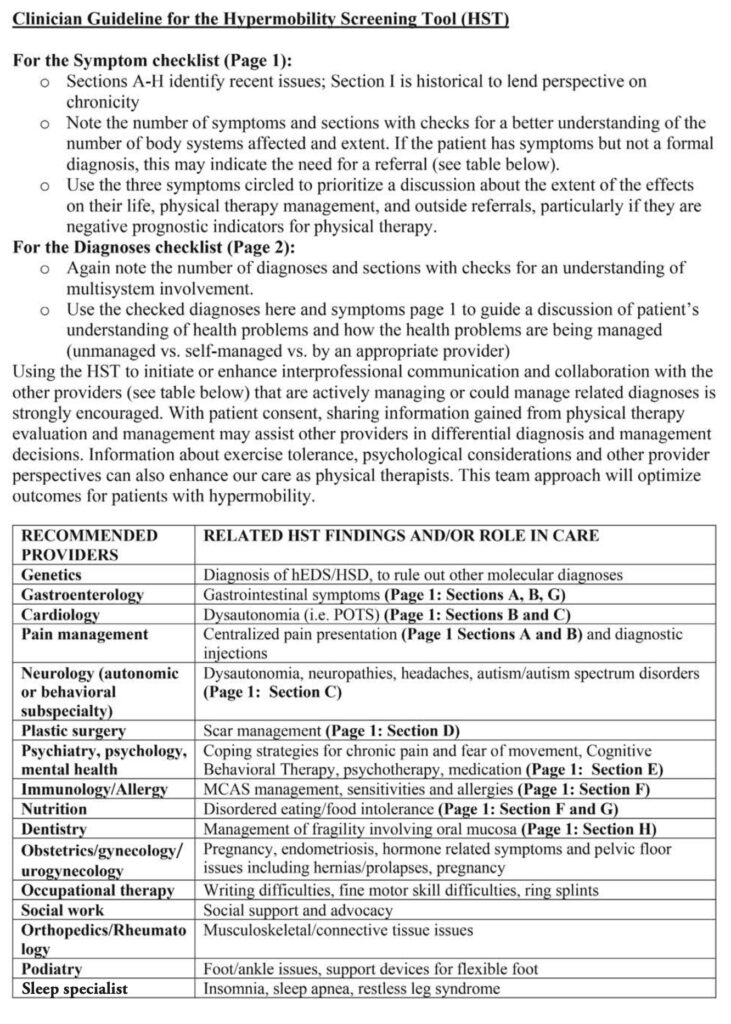
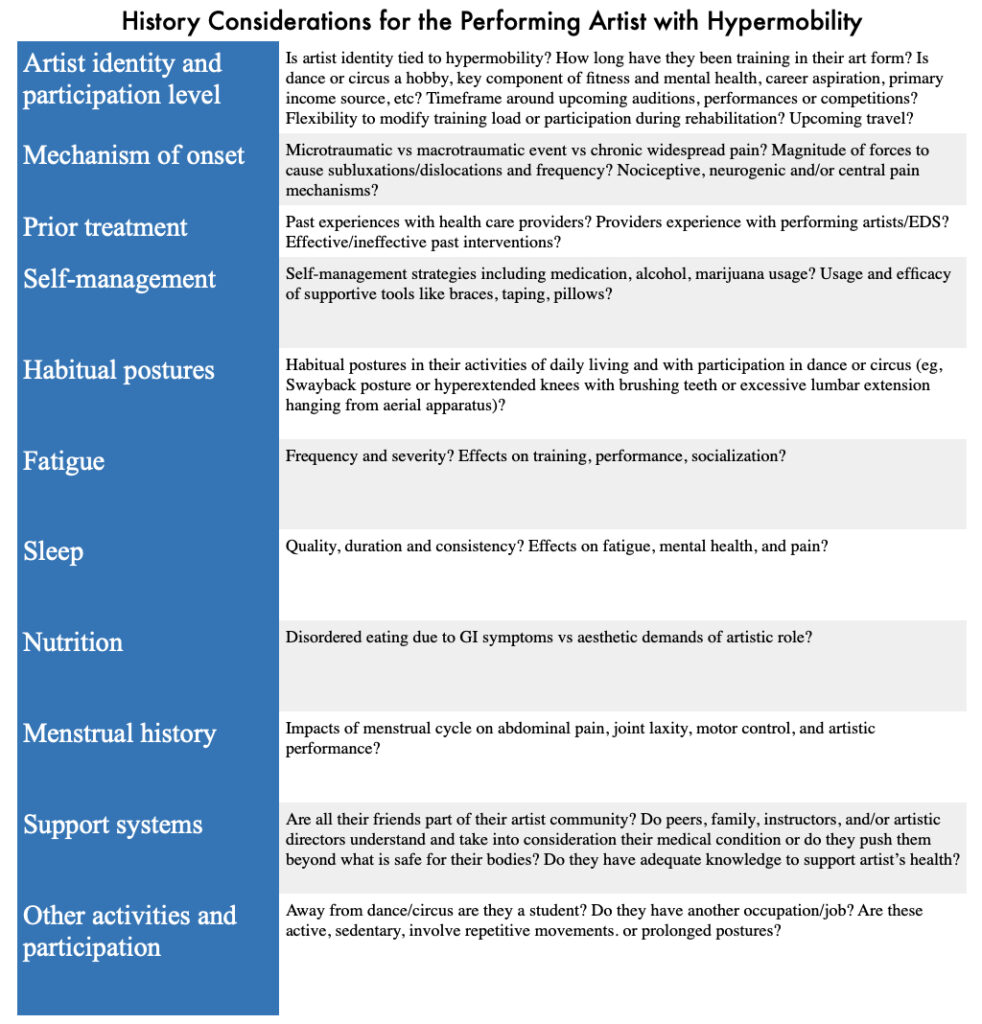
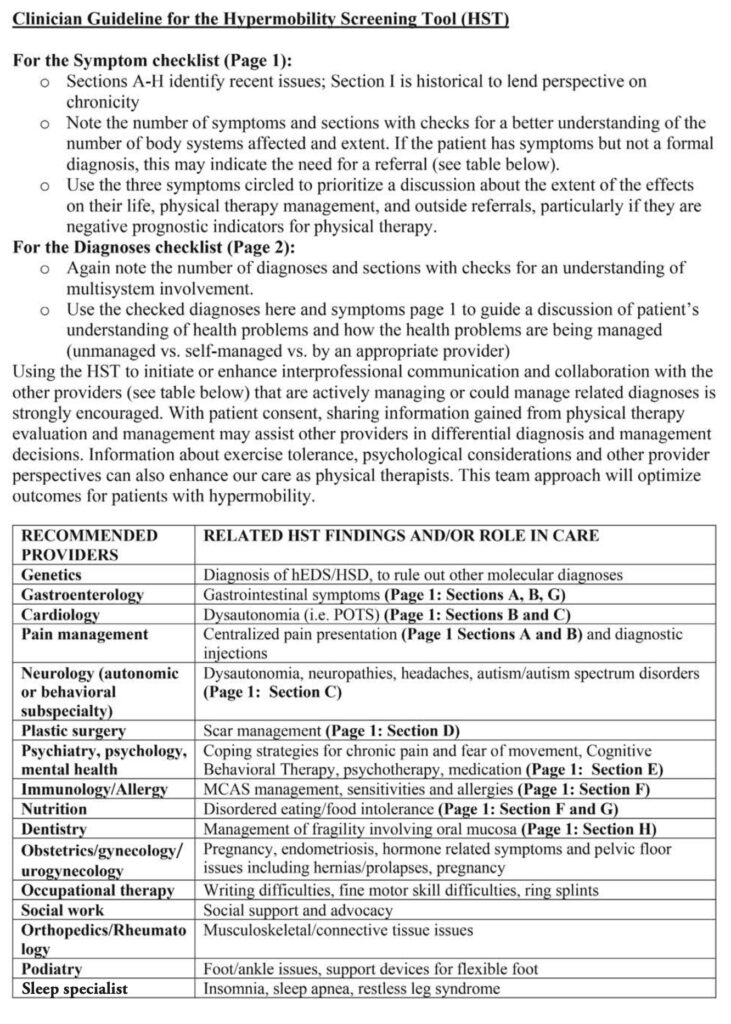
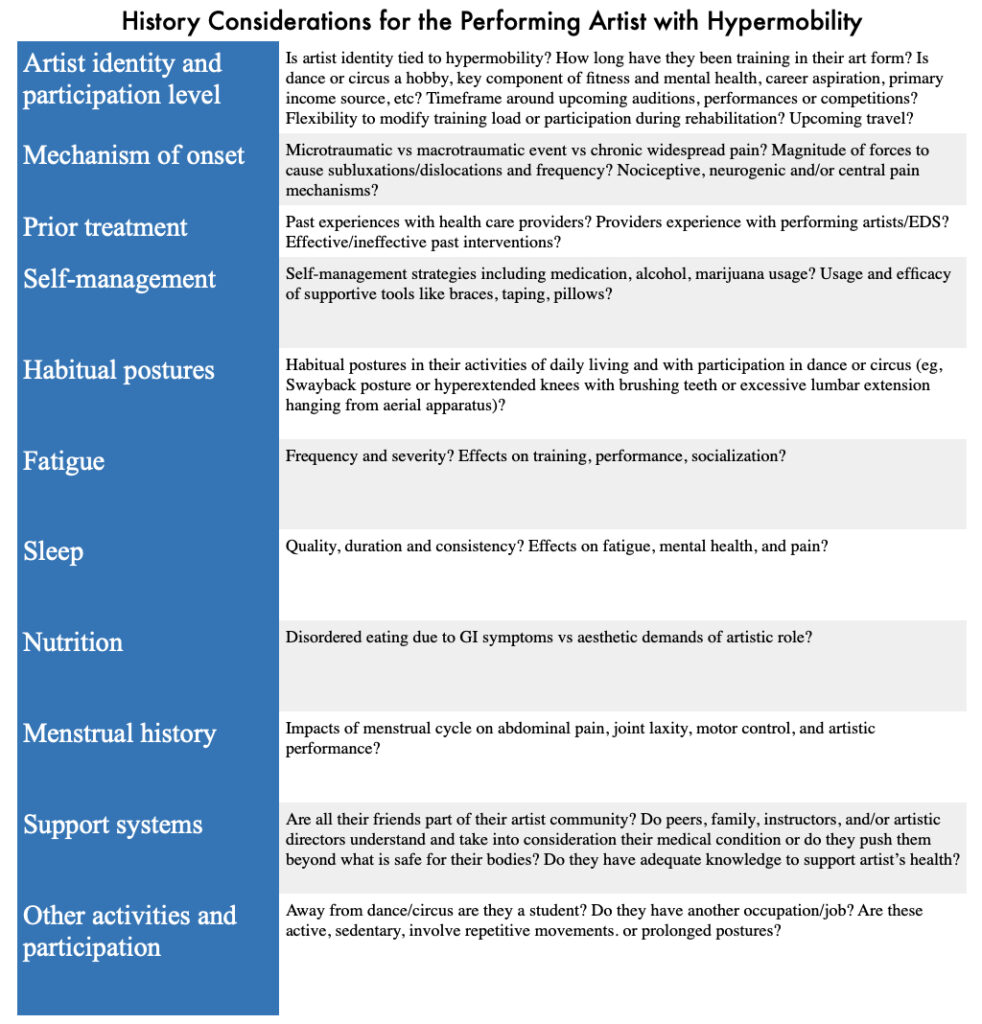
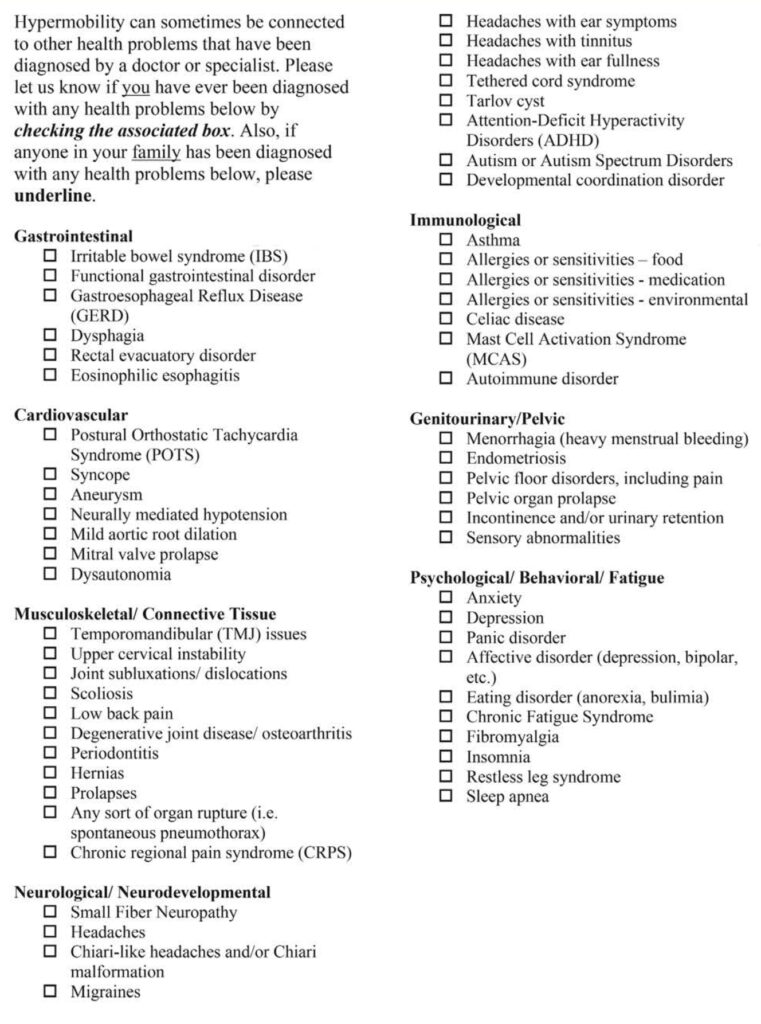
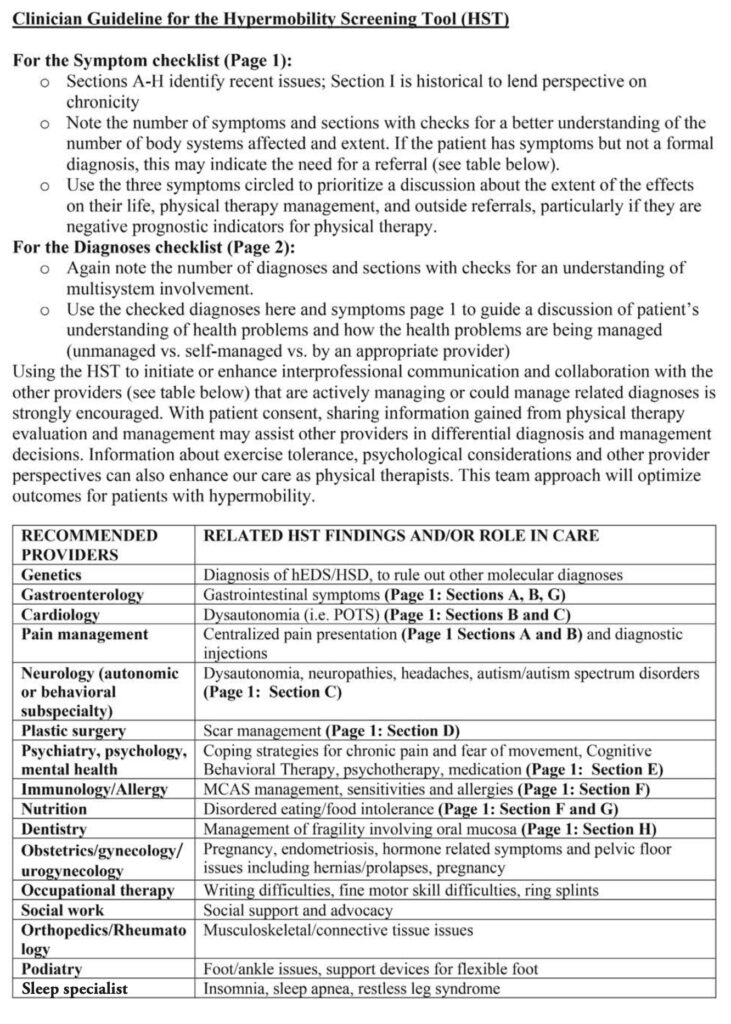
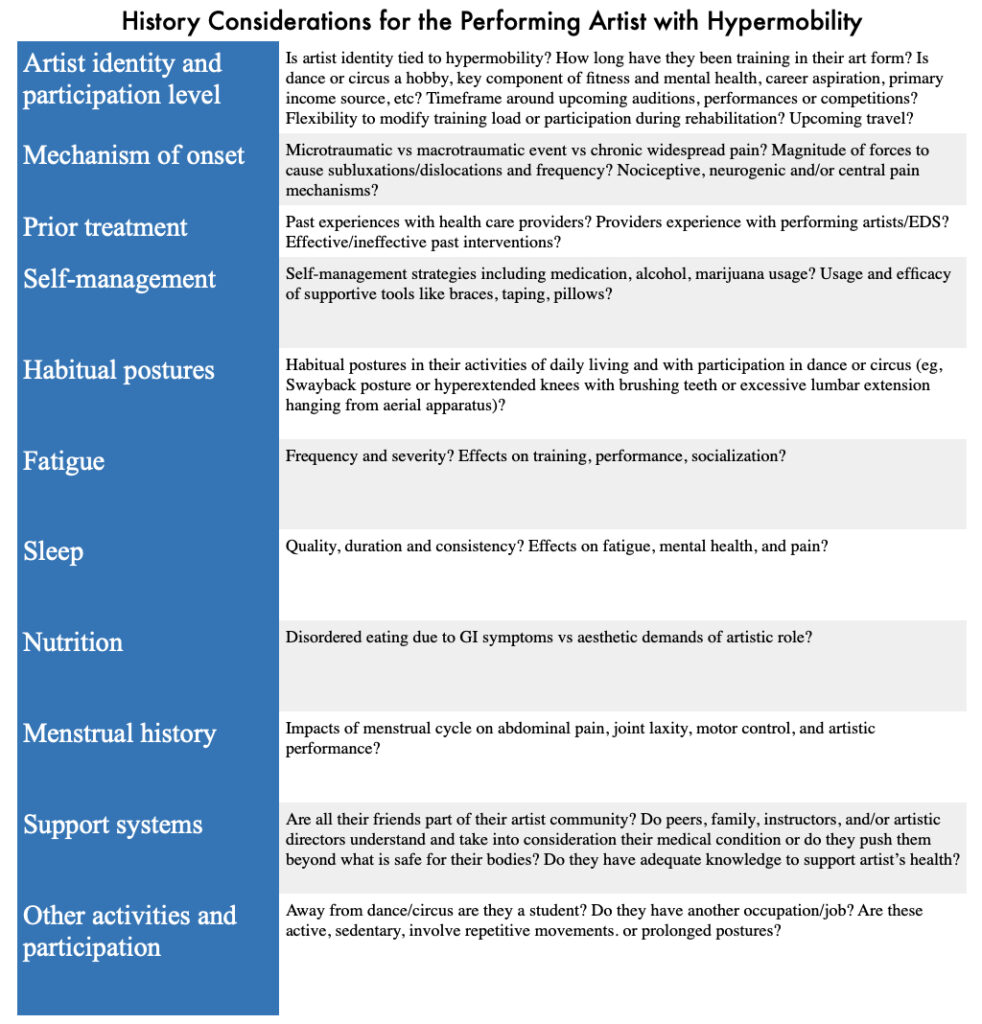
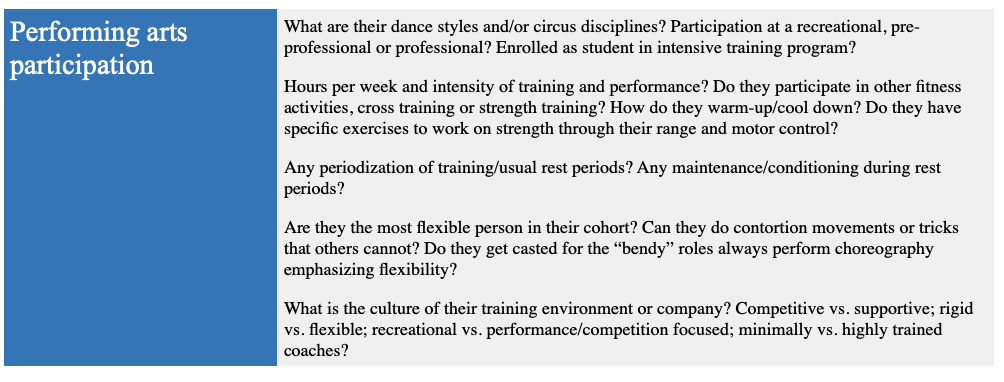
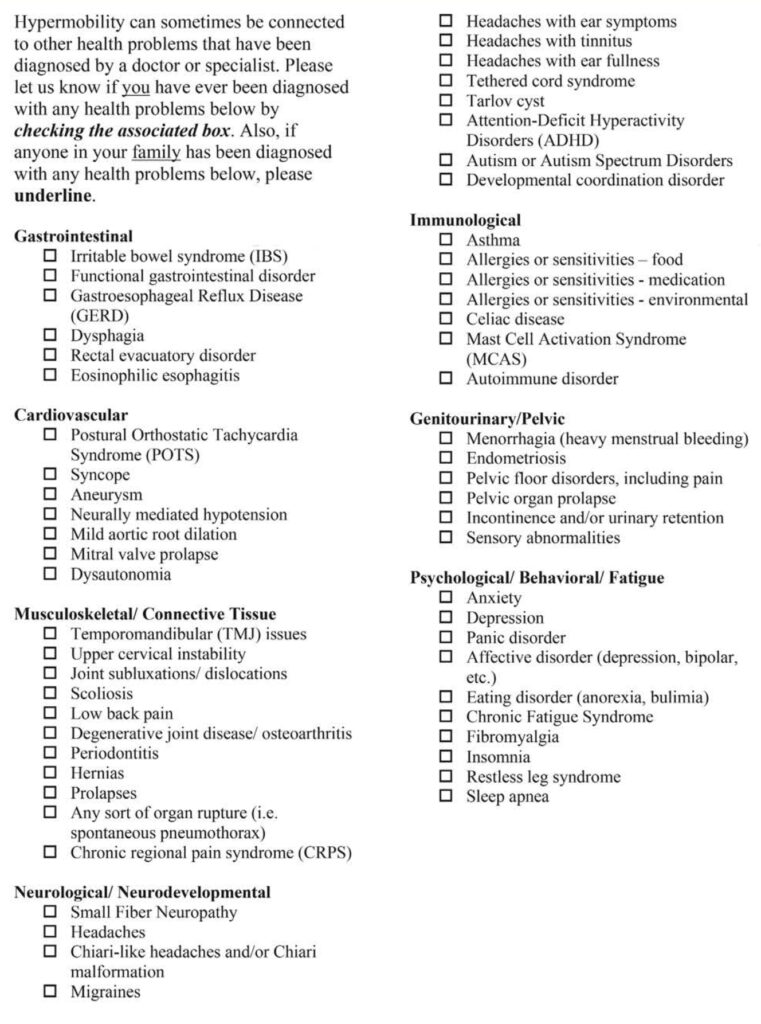
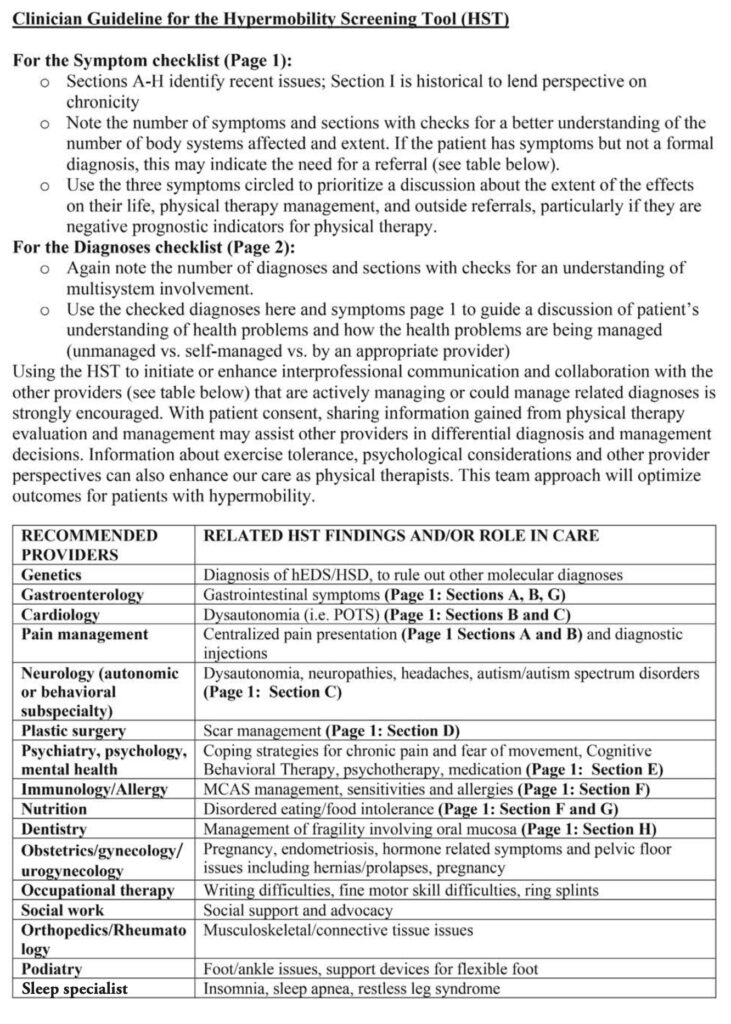
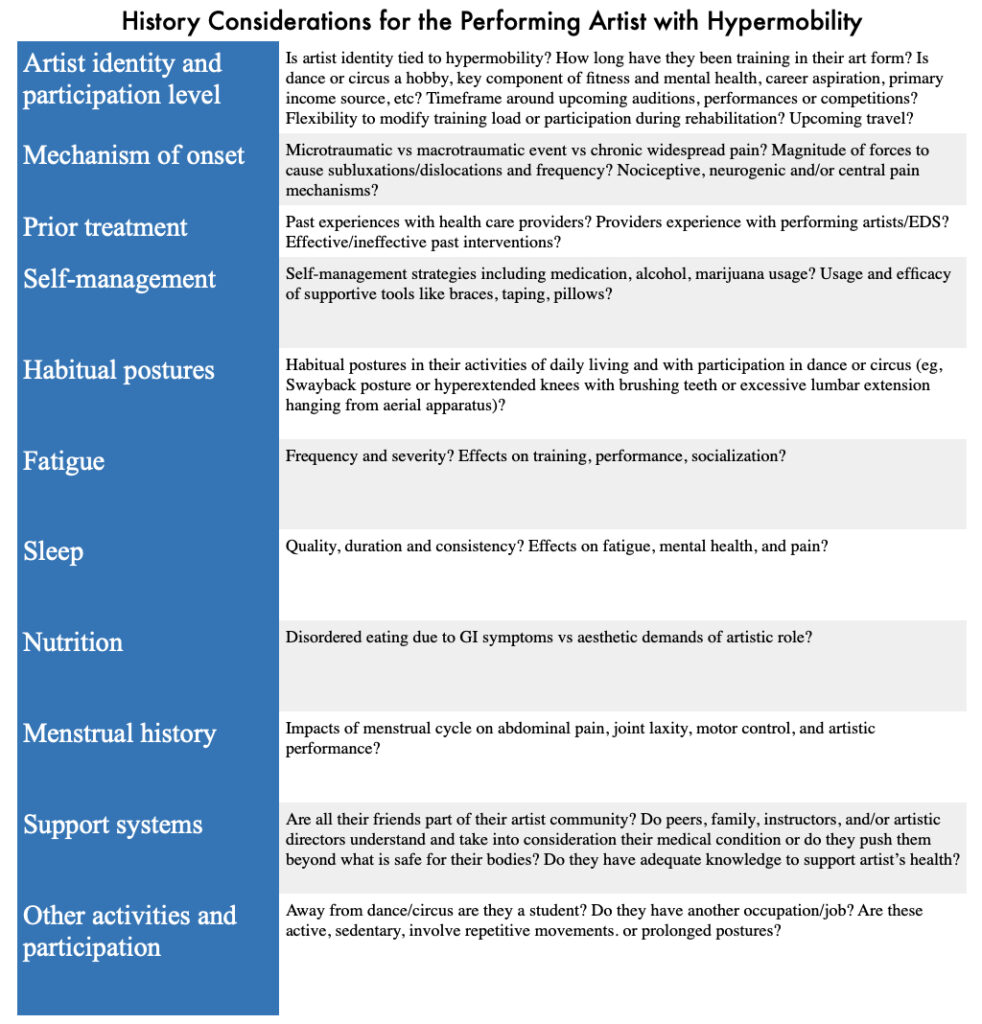
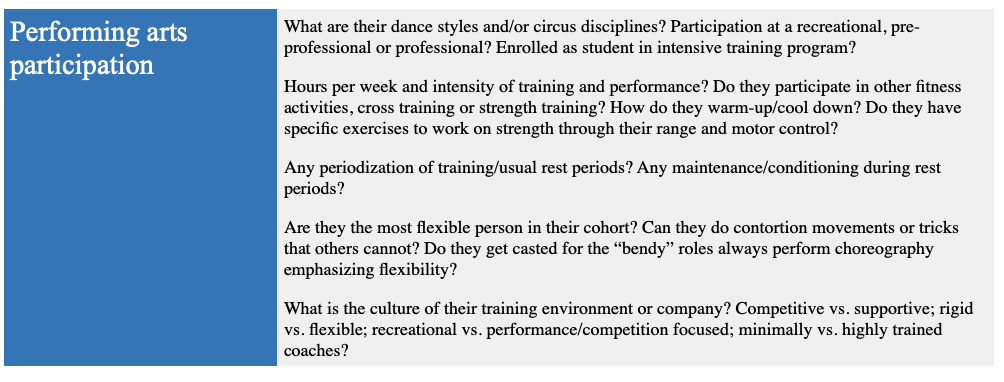
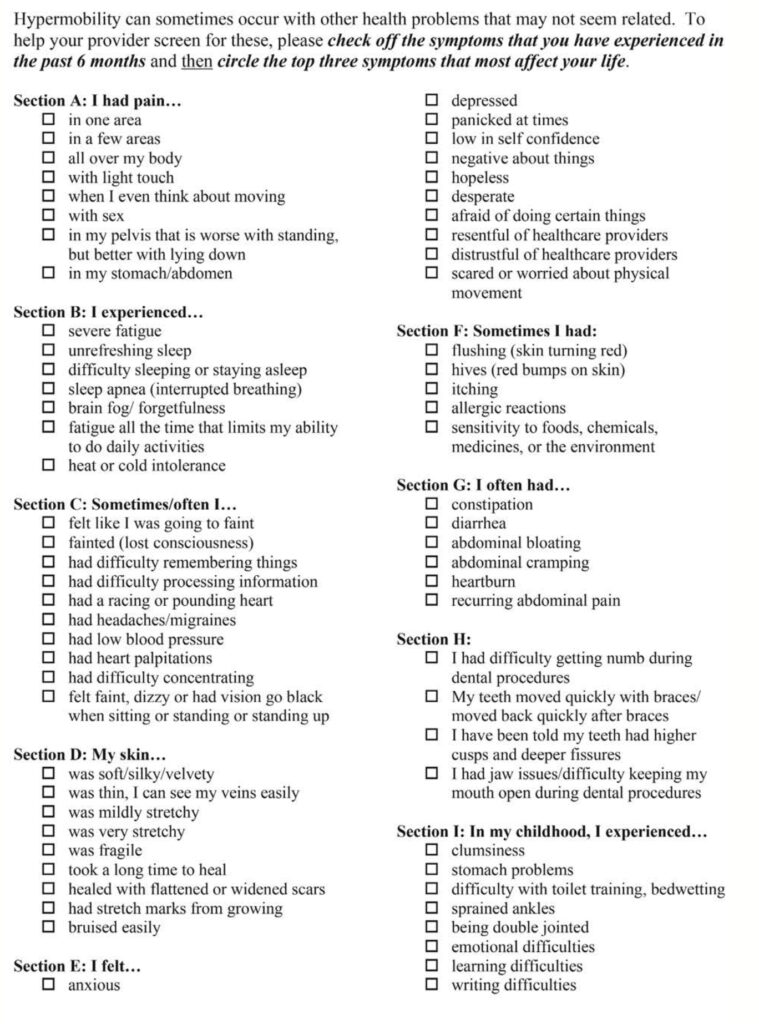
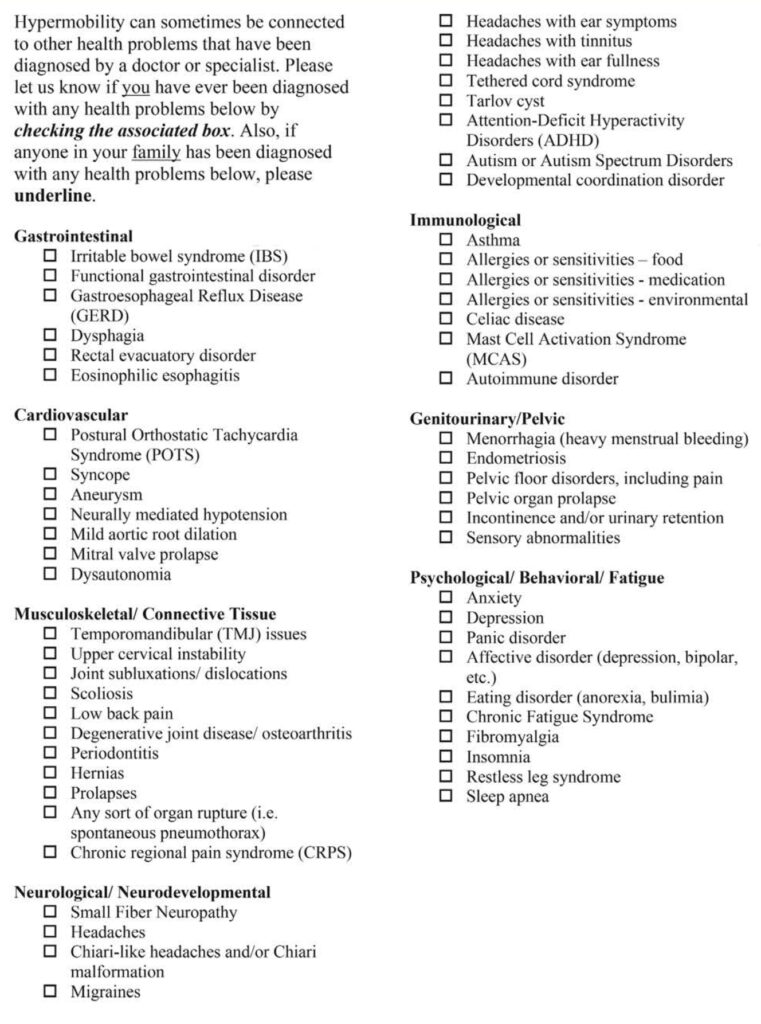
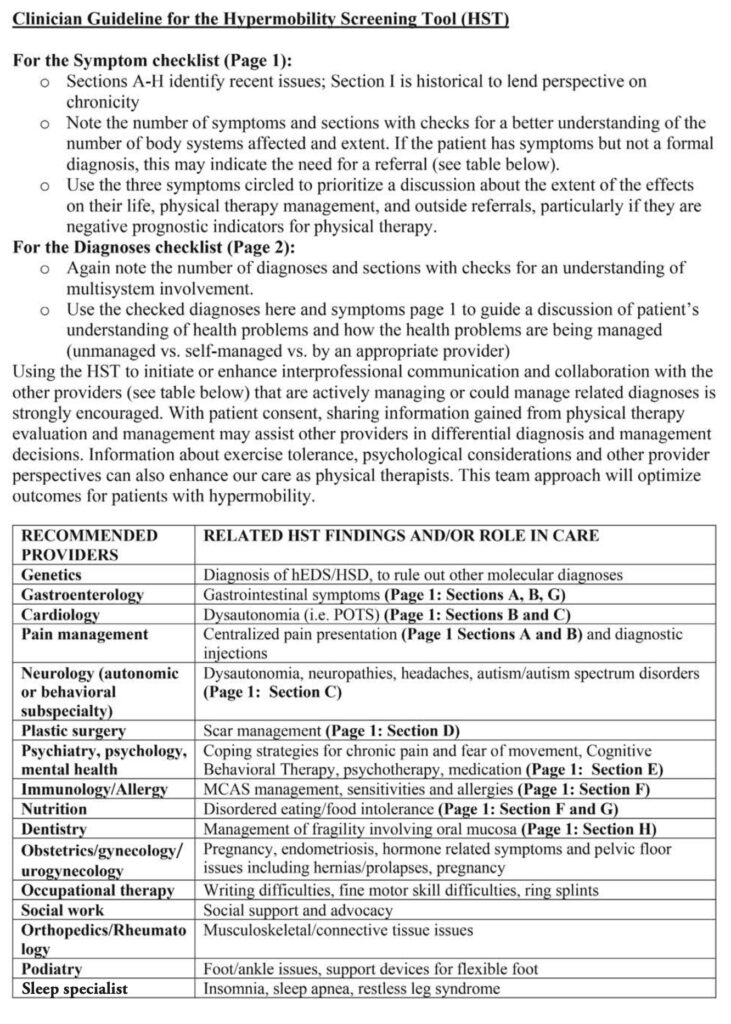
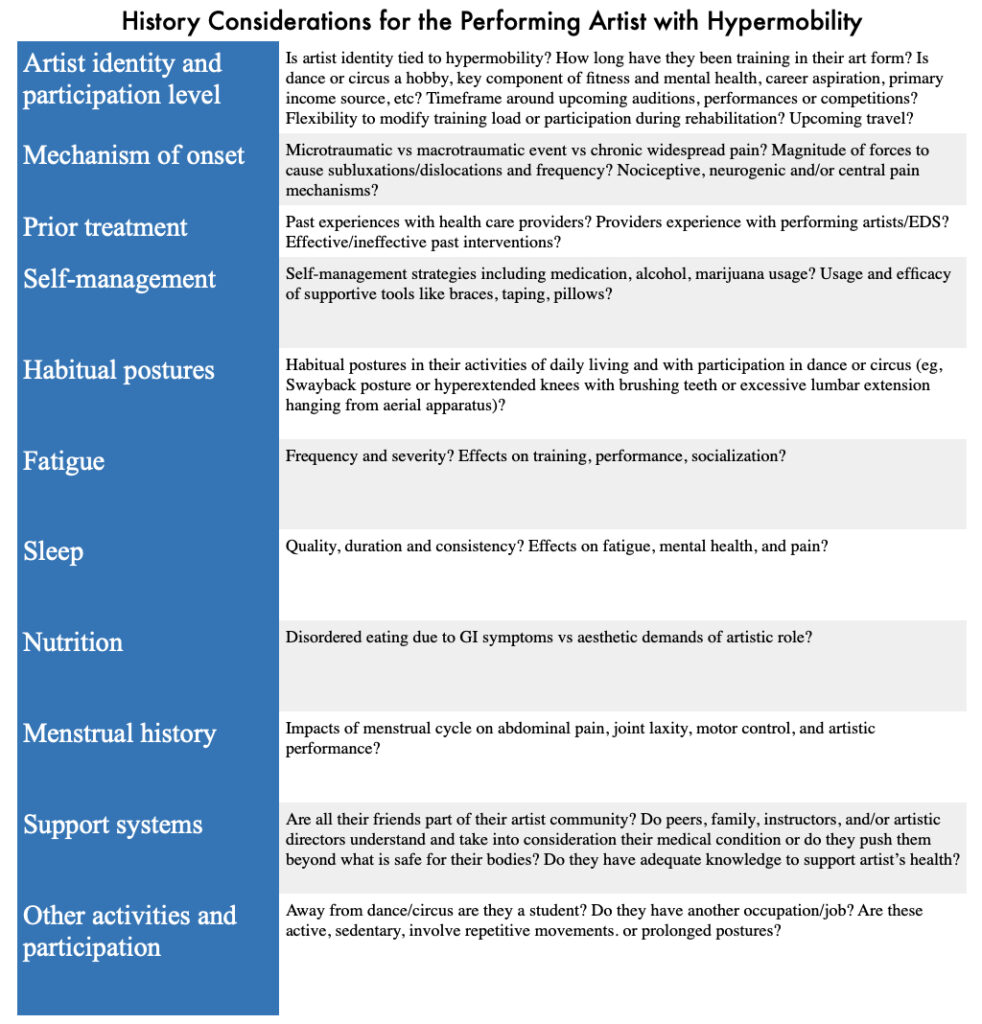
There are several physical and historical screens that a physical therapist can administer. The Hypermobility Screening Tool can assist therapists in identifying systems-related dysfunction, and allow for proper referral to a health care provider. For example, an athlete complaining of headaches or dizziness with changes in body position, or after participating in strenuous activity, may warrant referral to a cardiologist. An athlete reporting frequent ankle sprains may require referral to an orthopedic.
The Beighton Score, Brighton criteria and 5-point screening questionnaire can be used to screen for joint hypermobility. These scoring systems identify joints that have excessive flexibility. It helps physical therapists identify which body parts need continued observation or focused intervention to prevent an injury from occurring. Other tests may include muscle function (strength and endurance) and balance (joint stability plays an important role in posture).
Below is a chart describing the types of tests physical therapists can utilize to help athletes experiencing symptoms of EDS.

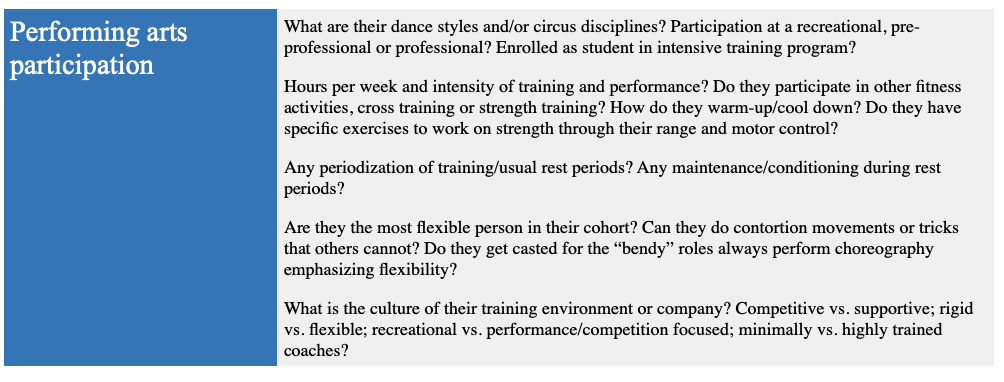
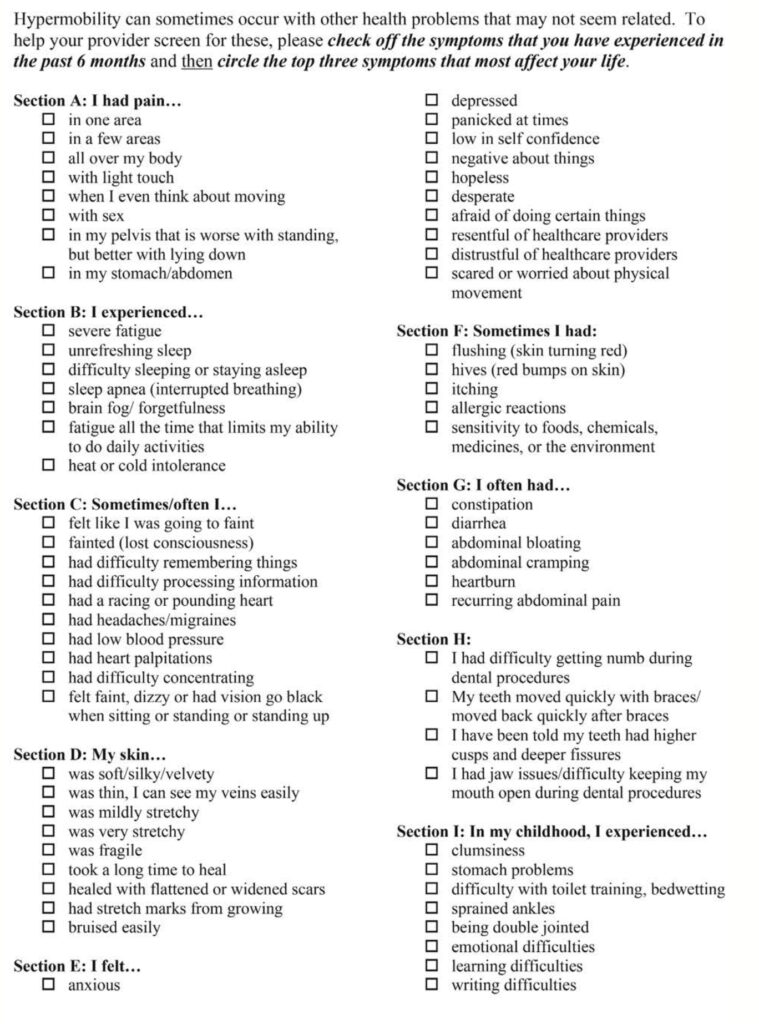
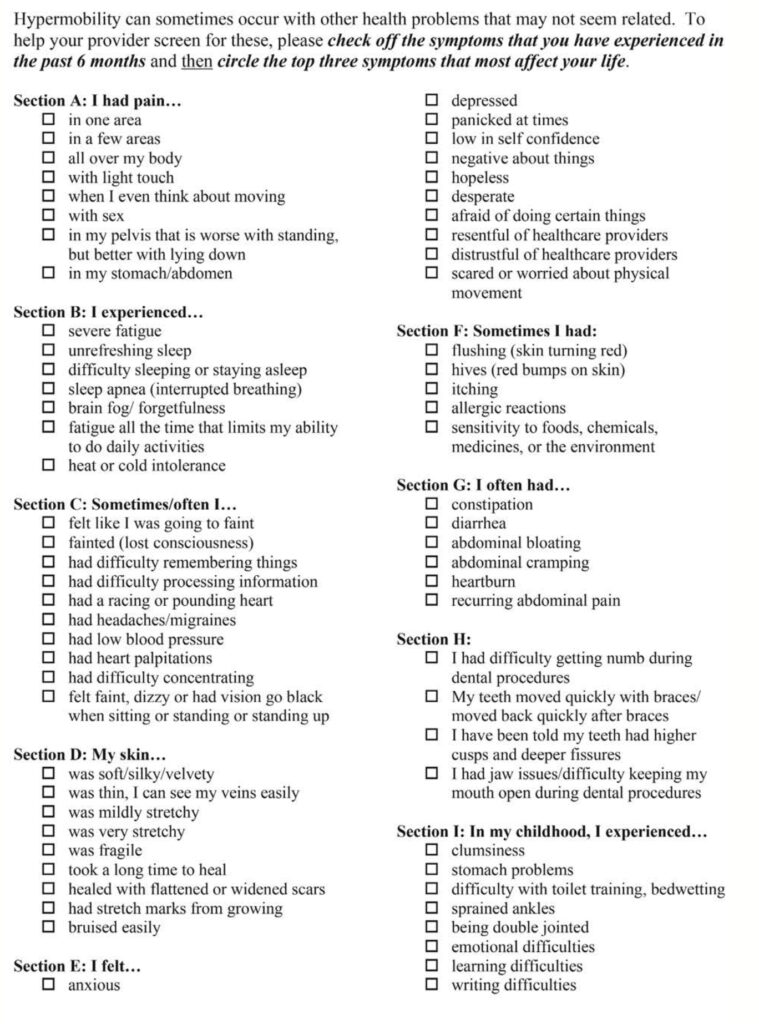
Athletes participating in sports that are seeking medical attention for pain or weakness often complete screening tools. These screening tools can help facilitate referral to a proper medical provider, or help direct treatment by a physical therapist. It also provides a kind of “journal” for an athlete to measure over a specific time period. By keeping record of the day and symptoms, an athlete can visualize over the course of treatment what their symptoms are at any given time frame.
Below is the screening tool.

Taken as a whole, athletes participating in sport that present with signs and symptoms suggestive of EDS or other hypermobile syndromes, should have a comprehensive evaluation including joint mobility, muscular strength, balance and coordination, in addition to systemic issues including gastrointestinal, cardiology, psychiatry and neurology. The relative muscular weakness of athletes presenting with EDS and hypermobile syndromes may require additional time or effort to improve strength to be able to perform well and reduce injury risk. The good news is that strength training has a protective effect on joints, improves pain experience and reduces the risk of fall-related injuries. It is imperative that the athlete and their trainers keep an eye on fatigue levels, as individuals with EDS tend to fatigue earlier compared to their non-EDS peers. If athletes with EDS are managing an injury, it is usually best to continue activity with modifications, rather than completely stop.
While EDS and hypermobile syndromes are highly prevalent in the performing arts community, awareness of the associated complications and injury-risk factors is not fully understood with all health care providers. Seeking physical therapy treatment from a therapist that understands the physical and emotional demands of performing arts in addition to complications with EDS can make an enormous difference in an athletes career.
If you are an athlete experiencing EDS or hypermobility, and are concerned about returning to sport, give our office a call. Dr. Abbate has years of experience helping hundreds of professional performing artists at Royal Caribbean and Celebrity Cruises. If he can help them, he can help you!
Pain is a very common experience for people with EDS. This can be due to joint subluxation, arthralgia (joint-related), myofascial (muscle, skin) and visceral (internal organs) pain. This may progress to sensitization of the central nervous system, or how the brain perceives the pain experience. There is a strong association of pain in EDS with depression and anxiety.
Engagement in early childhood may help offset the presentation of chronic pain, poor sleep, deconditioning, orthostatic intolerance and nutritional deficiencies typically seen in this population.
Excessive joint laxity, or flexibility, is a classic presentation of EDS. While aesthetically pleasing, it increases the risk of joint related pathology (hip, ankle and shoulder instability) and certain injuries (labral tears, tendinopathies and joint degeneration). This often leads to more time off to recover from injuries.
There are several physical and historical screens that a physical therapist can administer. The Hypermobility Screening Tool can assist therapists in identifying systems-related dysfunction, and allow for proper referral to a health care provider. For example, an athlete complaining of headaches or dizziness with changes in body position, or after participating in strenuous activity, may warrant referral to a cardiologist. An athlete reporting frequent ankle sprains may require referral to an orthopedic.
The Beighton Score, Brighton criteria and 5-point screening questionnaire can be used to screen for joint hypermobility. These scoring systems identify joints that have excessive flexibility. It helps physical therapists identify which body parts need continued observation or focused intervention to prevent an injury from occurring. Other tests may include muscle function (strength and endurance) and balance (joint stability plays an important role in posture).
Below is a chart describing the types of tests physical therapists can utilize to help athletes experiencing symptoms of EDS.

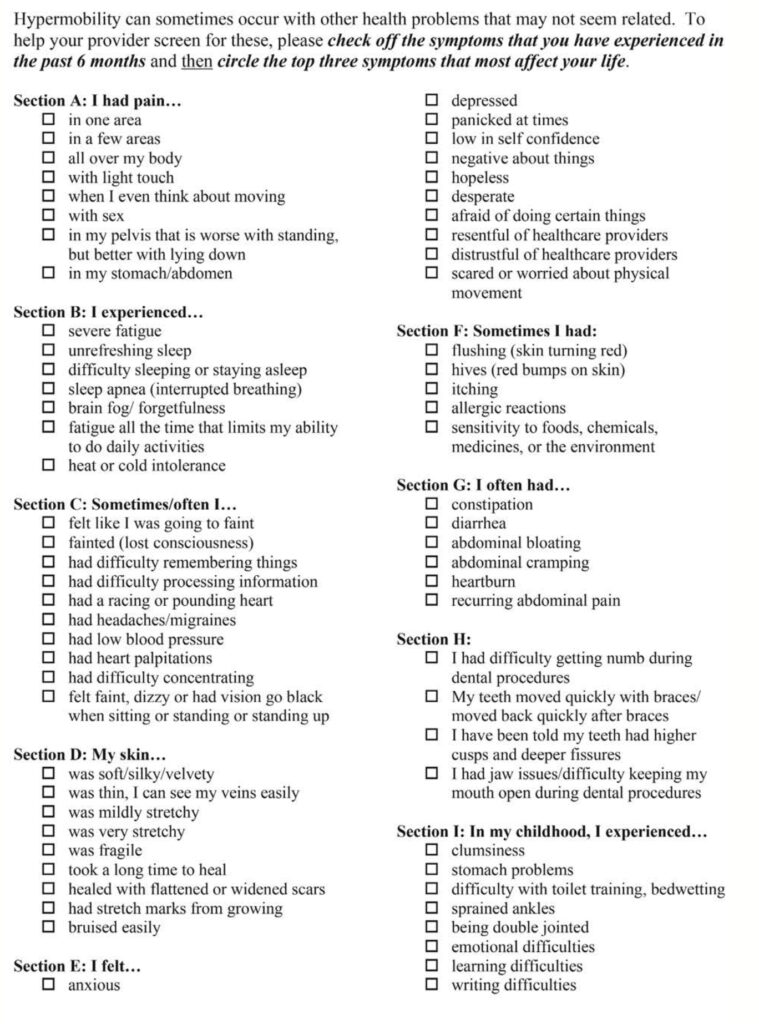
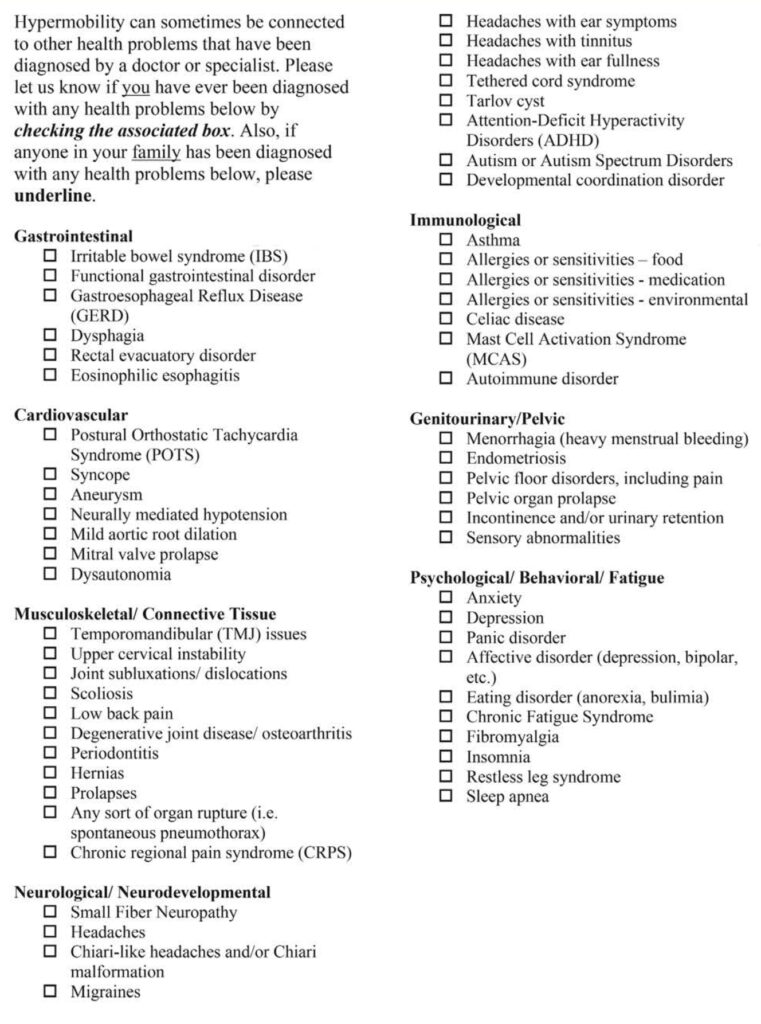
Athletes participating in sports that are seeking medical attention for pain or weakness often complete screening tools. These screening tools can help facilitate referral to a proper medical provider, or help direct treatment by a physical therapist. It also provides a kind of “journal” for an athlete to measure over a specific time period. By keeping record of the day and symptoms, an athlete can visualize over the course of treatment what their symptoms are at any given time frame.
Below is the screening tool.

Taken as a whole, athletes participating in sport that present with signs and symptoms suggestive of EDS or other hypermobile syndromes, should have a comprehensive evaluation including joint mobility, muscular strength, balance and coordination, in addition to systemic issues including gastrointestinal, cardiology, psychiatry and neurology. The relative muscular weakness of athletes presenting with EDS and hypermobile syndromes may require additional time or effort to improve strength to be able to perform well and reduce injury risk. The good news is that strength training has a protective effect on joints, improves pain experience and reduces the risk of fall-related injuries. It is imperative that the athlete and their trainers keep an eye on fatigue levels, as individuals with EDS tend to fatigue earlier compared to their non-EDS peers. If athletes with EDS are managing an injury, it is usually best to continue activity with modifications, rather than completely stop.
While EDS and hypermobile syndromes are highly prevalent in the performing arts community, awareness of the associated complications and injury-risk factors is not fully understood with all health care providers. Seeking physical therapy treatment from a therapist that understands the physical and emotional demands of performing arts in addition to complications with EDS can make an enormous difference in an athletes career.
If you are an athlete experiencing EDS or hypermobility, and are concerned about returning to sport, give our office a call. Dr. Abbate has years of experience helping hundreds of professional performing artists at Royal Caribbean and Celebrity Cruises. If he can help them, he can help you!
There are a number of health conditions associated with EDS. Poor blood pressure regulation, fatigue, headaches, anxiety and depression may be misinterpreted or downplayed by medical professionals.
Orthostatic intolerance (the ability for the body to maintain adequate blood pressure during or after activity) is present in about half of the population with EDS. Symptoms include dizziness, pre syncope, syncope, headaches, nausea, sweating or changes in blood pressure upon standing or after exercise.
Allergy-like symptoms of the skin (rashes), stomach (upset stomach), neuromuscular tissues (fatigue), airways (difficulty breathing), cardiovascular (abnormal heart rate response) and central nervous system (anxiety, depression) may appear at certain over an athletes career. Athletes may experience one or any combination of systemic issues. Nutritional deficiencies may present due to reflux, nausea, vomiting, irritable bowel syndrome, constipation and bloating. This may affect energy availability leading to fatigue and limiting tissue healing necessary after strenuous activity.
Pain is a very common experience for people with EDS. This can be due to joint subluxation, arthralgia (joint-related), myofascial (muscle, skin) and visceral (internal organs) pain. This may progress to sensitization of the central nervous system, or how the brain perceives the pain experience. There is a strong association of pain in EDS with depression and anxiety.
Engagement in early childhood may help offset the presentation of chronic pain, poor sleep, deconditioning, orthostatic intolerance and nutritional deficiencies typically seen in this population.
Excessive joint laxity, or flexibility, is a classic presentation of EDS. While aesthetically pleasing, it increases the risk of joint related pathology (hip, ankle and shoulder instability) and certain injuries (labral tears, tendinopathies and joint degeneration). This often leads to more time off to recover from injuries.
There are several physical and historical screens that a physical therapist can administer. The Hypermobility Screening Tool can assist therapists in identifying systems-related dysfunction, and allow for proper referral to a health care provider. For example, an athlete complaining of headaches or dizziness with changes in body position, or after participating in strenuous activity, may warrant referral to a cardiologist. An athlete reporting frequent ankle sprains may require referral to an orthopedic.
The Beighton Score, Brighton criteria and 5-point screening questionnaire can be used to screen for joint hypermobility. These scoring systems identify joints that have excessive flexibility. It helps physical therapists identify which body parts need continued observation or focused intervention to prevent an injury from occurring. Other tests may include muscle function (strength and endurance) and balance (joint stability plays an important role in posture).
Below is a chart describing the types of tests physical therapists can utilize to help athletes experiencing symptoms of EDS.

Athletes participating in sports that are seeking medical attention for pain or weakness often complete screening tools. These screening tools can help facilitate referral to a proper medical provider, or help direct treatment by a physical therapist. It also provides a kind of “journal” for an athlete to measure over a specific time period. By keeping record of the day and symptoms, an athlete can visualize over the course of treatment what their symptoms are at any given time frame.
Below is the screening tool.

Taken as a whole, athletes participating in sport that present with signs and symptoms suggestive of EDS or other hypermobile syndromes, should have a comprehensive evaluation including joint mobility, muscular strength, balance and coordination, in addition to systemic issues including gastrointestinal, cardiology, psychiatry and neurology. The relative muscular weakness of athletes presenting with EDS and hypermobile syndromes may require additional time or effort to improve strength to be able to perform well and reduce injury risk. The good news is that strength training has a protective effect on joints, improves pain experience and reduces the risk of fall-related injuries. It is imperative that the athlete and their trainers keep an eye on fatigue levels, as individuals with EDS tend to fatigue earlier compared to their non-EDS peers. If athletes with EDS are managing an injury, it is usually best to continue activity with modifications, rather than completely stop.
While EDS and hypermobile syndromes are highly prevalent in the performing arts community, awareness of the associated complications and injury-risk factors is not fully understood with all health care providers. Seeking physical therapy treatment from a therapist that understands the physical and emotional demands of performing arts in addition to complications with EDS can make an enormous difference in an athletes career.
If you are an athlete experiencing EDS or hypermobility, and are concerned about returning to sport, give our office a call. Dr. Abbate has years of experience helping hundreds of professional performing artists at Royal Caribbean and Celebrity Cruises. If he can help them, he can help you!
Secondary health complications due to connective tissue disorders include tendinopathy, joint subluxations/dislocations, scoliosis and arthritis. Additionally the autonomic, cardiovascular, skin and immune systems may be affected.
There are a number of health conditions associated with EDS. Poor blood pressure regulation, fatigue, headaches, anxiety and depression may be misinterpreted or downplayed by medical professionals.
Orthostatic intolerance (the ability for the body to maintain adequate blood pressure during or after activity) is present in about half of the population with EDS. Symptoms include dizziness, pre syncope, syncope, headaches, nausea, sweating or changes in blood pressure upon standing or after exercise.
Allergy-like symptoms of the skin (rashes), stomach (upset stomach), neuromuscular tissues (fatigue), airways (difficulty breathing), cardiovascular (abnormal heart rate response) and central nervous system (anxiety, depression) may appear at certain over an athletes career. Athletes may experience one or any combination of systemic issues. Nutritional deficiencies may present due to reflux, nausea, vomiting, irritable bowel syndrome, constipation and bloating. This may affect energy availability leading to fatigue and limiting tissue healing necessary after strenuous activity.
Pain is a very common experience for people with EDS. This can be due to joint subluxation, arthralgia (joint-related), myofascial (muscle, skin) and visceral (internal organs) pain. This may progress to sensitization of the central nervous system, or how the brain perceives the pain experience. There is a strong association of pain in EDS with depression and anxiety.
Engagement in early childhood may help offset the presentation of chronic pain, poor sleep, deconditioning, orthostatic intolerance and nutritional deficiencies typically seen in this population.
Excessive joint laxity, or flexibility, is a classic presentation of EDS. While aesthetically pleasing, it increases the risk of joint related pathology (hip, ankle and shoulder instability) and certain injuries (labral tears, tendinopathies and joint degeneration). This often leads to more time off to recover from injuries.
There are several physical and historical screens that a physical therapist can administer. The Hypermobility Screening Tool can assist therapists in identifying systems-related dysfunction, and allow for proper referral to a health care provider. For example, an athlete complaining of headaches or dizziness with changes in body position, or after participating in strenuous activity, may warrant referral to a cardiologist. An athlete reporting frequent ankle sprains may require referral to an orthopedic.
The Beighton Score, Brighton criteria and 5-point screening questionnaire can be used to screen for joint hypermobility. These scoring systems identify joints that have excessive flexibility. It helps physical therapists identify which body parts need continued observation or focused intervention to prevent an injury from occurring. Other tests may include muscle function (strength and endurance) and balance (joint stability plays an important role in posture).
Below is a chart describing the types of tests physical therapists can utilize to help athletes experiencing symptoms of EDS.

Athletes participating in sports that are seeking medical attention for pain or weakness often complete screening tools. These screening tools can help facilitate referral to a proper medical provider, or help direct treatment by a physical therapist. It also provides a kind of “journal” for an athlete to measure over a specific time period. By keeping record of the day and symptoms, an athlete can visualize over the course of treatment what their symptoms are at any given time frame.
Below is the screening tool.

Taken as a whole, athletes participating in sport that present with signs and symptoms suggestive of EDS or other hypermobile syndromes, should have a comprehensive evaluation including joint mobility, muscular strength, balance and coordination, in addition to systemic issues including gastrointestinal, cardiology, psychiatry and neurology. The relative muscular weakness of athletes presenting with EDS and hypermobile syndromes may require additional time or effort to improve strength to be able to perform well and reduce injury risk. The good news is that strength training has a protective effect on joints, improves pain experience and reduces the risk of fall-related injuries. It is imperative that the athlete and their trainers keep an eye on fatigue levels, as individuals with EDS tend to fatigue earlier compared to their non-EDS peers. If athletes with EDS are managing an injury, it is usually best to continue activity with modifications, rather than completely stop.
While EDS and hypermobile syndromes are highly prevalent in the performing arts community, awareness of the associated complications and injury-risk factors is not fully understood with all health care providers. Seeking physical therapy treatment from a therapist that understands the physical and emotional demands of performing arts in addition to complications with EDS can make an enormous difference in an athletes career.
If you are an athlete experiencing EDS or hypermobility, and are concerned about returning to sport, give our office a call. Dr. Abbate has years of experience helping hundreds of professional performing artists at Royal Caribbean and Celebrity Cruises. If he can help them, he can help you!
Secondary health complications due to connective tissue disorders include tendinopathy, joint subluxations/dislocations, scoliosis and arthritis. Additionally the autonomic, cardiovascular, skin and immune systems may be affected.
There are a number of health conditions associated with EDS. Poor blood pressure regulation, fatigue, headaches, anxiety and depression may be misinterpreted or downplayed by medical professionals.
Orthostatic intolerance (the ability for the body to maintain adequate blood pressure during or after activity) is present in about half of the population with EDS. Symptoms include dizziness, pre syncope, syncope, headaches, nausea, sweating or changes in blood pressure upon standing or after exercise.
Allergy-like symptoms of the skin (rashes), stomach (upset stomach), neuromuscular tissues (fatigue), airways (difficulty breathing), cardiovascular (abnormal heart rate response) and central nervous system (anxiety, depression) may appear at certain over an athletes career. Athletes may experience one or any combination of systemic issues. Nutritional deficiencies may present due to reflux, nausea, vomiting, irritable bowel syndrome, constipation and bloating. This may affect energy availability leading to fatigue and limiting tissue healing necessary after strenuous activity.
Pain is a very common experience for people with EDS. This can be due to joint subluxation, arthralgia (joint-related), myofascial (muscle, skin) and visceral (internal organs) pain. This may progress to sensitization of the central nervous system, or how the brain perceives the pain experience. There is a strong association of pain in EDS with depression and anxiety.
Engagement in early childhood may help offset the presentation of chronic pain, poor sleep, deconditioning, orthostatic intolerance and nutritional deficiencies typically seen in this population.
Excessive joint laxity, or flexibility, is a classic presentation of EDS. While aesthetically pleasing, it increases the risk of joint related pathology (hip, ankle and shoulder instability) and certain injuries (labral tears, tendinopathies and joint degeneration). This often leads to more time off to recover from injuries.
There are several physical and historical screens that a physical therapist can administer. The Hypermobility Screening Tool can assist therapists in identifying systems-related dysfunction, and allow for proper referral to a health care provider. For example, an athlete complaining of headaches or dizziness with changes in body position, or after participating in strenuous activity, may warrant referral to a cardiologist. An athlete reporting frequent ankle sprains may require referral to an orthopedic.
The Beighton Score, Brighton criteria and 5-point screening questionnaire can be used to screen for joint hypermobility. These scoring systems identify joints that have excessive flexibility. It helps physical therapists identify which body parts need continued observation or focused intervention to prevent an injury from occurring. Other tests may include muscle function (strength and endurance) and balance (joint stability plays an important role in posture).
Below is a chart describing the types of tests physical therapists can utilize to help athletes experiencing symptoms of EDS.

Athletes participating in sports that are seeking medical attention for pain or weakness often complete screening tools. These screening tools can help facilitate referral to a proper medical provider, or help direct treatment by a physical therapist. It also provides a kind of “journal” for an athlete to measure over a specific time period. By keeping record of the day and symptoms, an athlete can visualize over the course of treatment what their symptoms are at any given time frame.
Below is the screening tool.

Taken as a whole, athletes participating in sport that present with signs and symptoms suggestive of EDS or other hypermobile syndromes, should have a comprehensive evaluation including joint mobility, muscular strength, balance and coordination, in addition to systemic issues including gastrointestinal, cardiology, psychiatry and neurology. The relative muscular weakness of athletes presenting with EDS and hypermobile syndromes may require additional time or effort to improve strength to be able to perform well and reduce injury risk. The good news is that strength training has a protective effect on joints, improves pain experience and reduces the risk of fall-related injuries. It is imperative that the athlete and their trainers keep an eye on fatigue levels, as individuals with EDS tend to fatigue earlier compared to their non-EDS peers. If athletes with EDS are managing an injury, it is usually best to continue activity with modifications, rather than completely stop.
While EDS and hypermobile syndromes are highly prevalent in the performing arts community, awareness of the associated complications and injury-risk factors is not fully understood with all health care providers. Seeking physical therapy treatment from a therapist that understands the physical and emotional demands of performing arts in addition to complications with EDS can make an enormous difference in an athletes career.
If you are an athlete experiencing EDS or hypermobility, and are concerned about returning to sport, give our office a call. Dr. Abbate has years of experience helping hundreds of professional performing artists at Royal Caribbean and Celebrity Cruises. If he can help them, he can help you!
The International Consortium on the Ehlers-Danlos Syndromes defined the following diagnostic criteria:
Secondary health complications due to connective tissue disorders include tendinopathy, joint subluxations/dislocations, scoliosis and arthritis. Additionally the autonomic, cardiovascular, skin and immune systems may be affected.
There are a number of health conditions associated with EDS. Poor blood pressure regulation, fatigue, headaches, anxiety and depression may be misinterpreted or downplayed by medical professionals.
Orthostatic intolerance (the ability for the body to maintain adequate blood pressure during or after activity) is present in about half of the population with EDS. Symptoms include dizziness, pre syncope, syncope, headaches, nausea, sweating or changes in blood pressure upon standing or after exercise.
Allergy-like symptoms of the skin (rashes), stomach (upset stomach), neuromuscular tissues (fatigue), airways (difficulty breathing), cardiovascular (abnormal heart rate response) and central nervous system (anxiety, depression) may appear at certain over an athletes career. Athletes may experience one or any combination of systemic issues. Nutritional deficiencies may present due to reflux, nausea, vomiting, irritable bowel syndrome, constipation and bloating. This may affect energy availability leading to fatigue and limiting tissue healing necessary after strenuous activity.
Pain is a very common experience for people with EDS. This can be due to joint subluxation, arthralgia (joint-related), myofascial (muscle, skin) and visceral (internal organs) pain. This may progress to sensitization of the central nervous system, or how the brain perceives the pain experience. There is a strong association of pain in EDS with depression and anxiety.
Engagement in early childhood may help offset the presentation of chronic pain, poor sleep, deconditioning, orthostatic intolerance and nutritional deficiencies typically seen in this population.
Excessive joint laxity, or flexibility, is a classic presentation of EDS. While aesthetically pleasing, it increases the risk of joint related pathology (hip, ankle and shoulder instability) and certain injuries (labral tears, tendinopathies and joint degeneration). This often leads to more time off to recover from injuries.
There are several physical and historical screens that a physical therapist can administer. The Hypermobility Screening Tool can assist therapists in identifying systems-related dysfunction, and allow for proper referral to a health care provider. For example, an athlete complaining of headaches or dizziness with changes in body position, or after participating in strenuous activity, may warrant referral to a cardiologist. An athlete reporting frequent ankle sprains may require referral to an orthopedic.
The Beighton Score, Brighton criteria and 5-point screening questionnaire can be used to screen for joint hypermobility. These scoring systems identify joints that have excessive flexibility. It helps physical therapists identify which body parts need continued observation or focused intervention to prevent an injury from occurring. Other tests may include muscle function (strength and endurance) and balance (joint stability plays an important role in posture).
Below is a chart describing the types of tests physical therapists can utilize to help athletes experiencing symptoms of EDS.

Athletes participating in sports that are seeking medical attention for pain or weakness often complete screening tools. These screening tools can help facilitate referral to a proper medical provider, or help direct treatment by a physical therapist. It also provides a kind of “journal” for an athlete to measure over a specific time period. By keeping record of the day and symptoms, an athlete can visualize over the course of treatment what their symptoms are at any given time frame.
Below is the screening tool.

Taken as a whole, athletes participating in sport that present with signs and symptoms suggestive of EDS or other hypermobile syndromes, should have a comprehensive evaluation including joint mobility, muscular strength, balance and coordination, in addition to systemic issues including gastrointestinal, cardiology, psychiatry and neurology. The relative muscular weakness of athletes presenting with EDS and hypermobile syndromes may require additional time or effort to improve strength to be able to perform well and reduce injury risk. The good news is that strength training has a protective effect on joints, improves pain experience and reduces the risk of fall-related injuries. It is imperative that the athlete and their trainers keep an eye on fatigue levels, as individuals with EDS tend to fatigue earlier compared to their non-EDS peers. If athletes with EDS are managing an injury, it is usually best to continue activity with modifications, rather than completely stop.
While EDS and hypermobile syndromes are highly prevalent in the performing arts community, awareness of the associated complications and injury-risk factors is not fully understood with all health care providers. Seeking physical therapy treatment from a therapist that understands the physical and emotional demands of performing arts in addition to complications with EDS can make an enormous difference in an athletes career.
If you are an athlete experiencing EDS or hypermobility, and are concerned about returning to sport, give our office a call. Dr. Abbate has years of experience helping hundreds of professional performing artists at Royal Caribbean and Celebrity Cruises. If he can help them, he can help you!

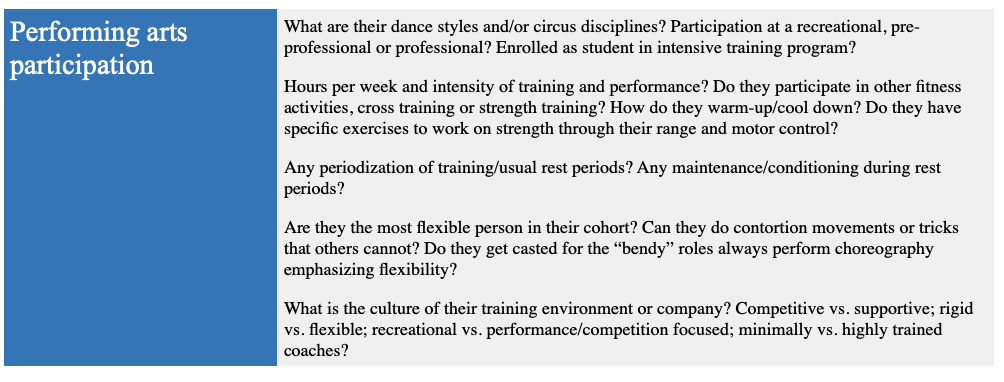
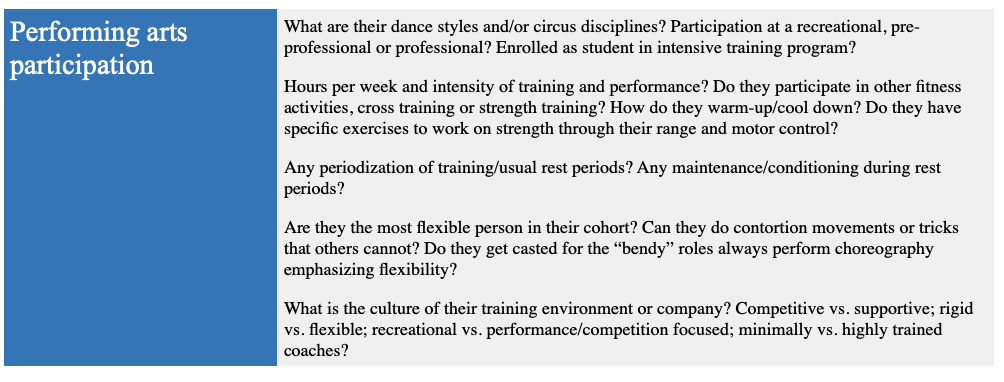
This article will describe joint hypermobility in the performing artist. I will discuss the importance of flexibility in the sports, the prevalence of specific hypermobility syndromes, how they are diagnosed, health related problems and injury risk and finally the role and relationship of physical therapy in the management of hypermobility.
Like most other athletic endeavors, there are changes in the aesthetic nature of the performing arts. The competitive demands of the sport, coupled with more demanding audiences for the “extreme” has caused an evolution in technique and thus performance. Flexibility specifically, has dramatically increased in performing artists across the spectrum over the past century. Aerialists, acrobats, dancers and contortionists are under constant pressure to take their skill to the next level. Athletes are performing more complex and physically demanding activities at younger ages.
Lets discuss joint hypermobility, a condition that gives athletes extreme flexibility. Hypermobility is defined as “the capability of a joint(s) to move past their normal limits”. This is often achieved by spending countless hours stretching over an athletes career. For some athletes, however, hypermobility is due to connective tissue disorders such as Ehlers-Danlos Syndrome (EDS). Ehlers-Danlos is present between 1-3% of the general population, or about 10 million people in the United States. In elite ballet dancers, between 74-95% have EDS. While EDS allows for beautiful “lines” when performing, there are a number of serious health complications associated with this condition. Given the significant percentage of dancers with EDS, it is imperative for performing artists and health care professionals to understand this condition and how to manage it.
The International Consortium on the Ehlers-Danlos Syndromes defined the following diagnostic criteria:
Secondary health complications due to connective tissue disorders include tendinopathy, joint subluxations/dislocations, scoliosis and arthritis. Additionally the autonomic, cardiovascular, skin and immune systems may be affected.
There are a number of health conditions associated with EDS. Poor blood pressure regulation, fatigue, headaches, anxiety and depression may be misinterpreted or downplayed by medical professionals.
Orthostatic intolerance (the ability for the body to maintain adequate blood pressure during or after activity) is present in about half of the population with EDS. Symptoms include dizziness, pre syncope, syncope, headaches, nausea, sweating or changes in blood pressure upon standing or after exercise.
Allergy-like symptoms of the skin (rashes), stomach (upset stomach), neuromuscular tissues (fatigue), airways (difficulty breathing), cardiovascular (abnormal heart rate response) and central nervous system (anxiety, depression) may appear at certain over an athletes career. Athletes may experience one or any combination of systemic issues. Nutritional deficiencies may present due to reflux, nausea, vomiting, irritable bowel syndrome, constipation and bloating. This may affect energy availability leading to fatigue and limiting tissue healing necessary after strenuous activity.
Pain is a very common experience for people with EDS. This can be due to joint subluxation, arthralgia (joint-related), myofascial (muscle, skin) and visceral (internal organs) pain. This may progress to sensitization of the central nervous system, or how the brain perceives the pain experience. There is a strong association of pain in EDS with depression and anxiety.
Engagement in early childhood may help offset the presentation of chronic pain, poor sleep, deconditioning, orthostatic intolerance and nutritional deficiencies typically seen in this population.
Excessive joint laxity, or flexibility, is a classic presentation of EDS. While aesthetically pleasing, it increases the risk of joint related pathology (hip, ankle and shoulder instability) and certain injuries (labral tears, tendinopathies and joint degeneration). This often leads to more time off to recover from injuries.
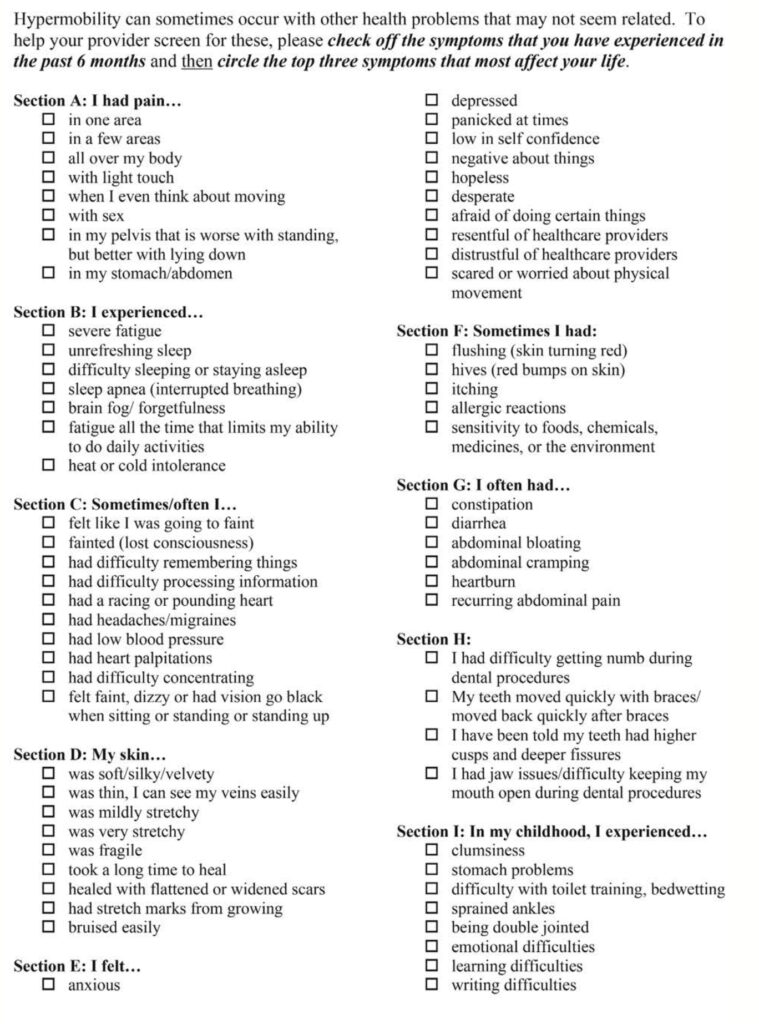
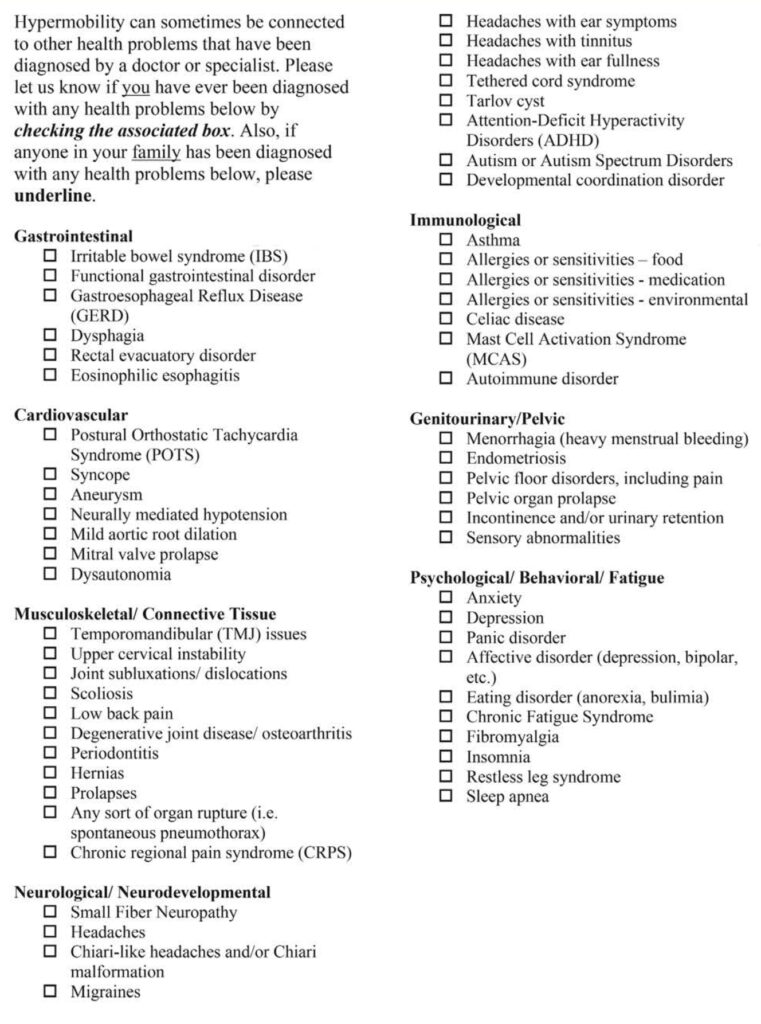
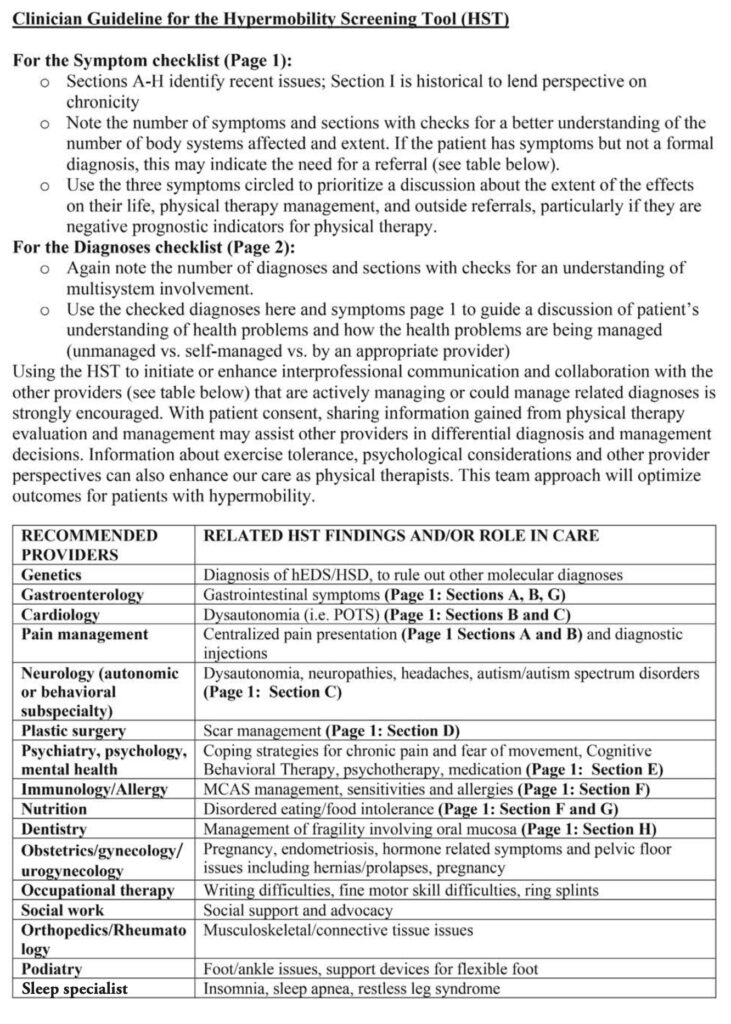
There are several physical and historical screens that a physical therapist can administer. The Hypermobility Screening Tool can assist therapists in identifying systems-related dysfunction, and allow for proper referral to a health care provider. For example, an athlete complaining of headaches or dizziness with changes in body position, or after participating in strenuous activity, may warrant referral to a cardiologist. An athlete reporting frequent ankle sprains may require referral to an orthopedic.
The Beighton Score, Brighton criteria and 5-point screening questionnaire can be used to screen for joint hypermobility. These scoring systems identify joints that have excessive flexibility. It helps physical therapists identify which body parts need continued observation or focused intervention to prevent an injury from occurring. Other tests may include muscle function (strength and endurance) and balance (joint stability plays an important role in posture).
Below is a chart describing the types of tests physical therapists can utilize to help athletes experiencing symptoms of EDS.

Athletes participating in sports that are seeking medical attention for pain or weakness often complete screening tools. These screening tools can help facilitate referral to a proper medical provider, or help direct treatment by a physical therapist. It also provides a kind of “journal” for an athlete to measure over a specific time period. By keeping record of the day and symptoms, an athlete can visualize over the course of treatment what their symptoms are at any given time frame.
Below is the screening tool.

Taken as a whole, athletes participating in sport that present with signs and symptoms suggestive of EDS or other hypermobile syndromes, should have a comprehensive evaluation including joint mobility, muscular strength, balance and coordination, in addition to systemic issues including gastrointestinal, cardiology, psychiatry and neurology. The relative muscular weakness of athletes presenting with EDS and hypermobile syndromes may require additional time or effort to improve strength to be able to perform well and reduce injury risk. The good news is that strength training has a protective effect on joints, improves pain experience and reduces the risk of fall-related injuries. It is imperative that the athlete and their trainers keep an eye on fatigue levels, as individuals with EDS tend to fatigue earlier compared to their non-EDS peers. If athletes with EDS are managing an injury, it is usually best to continue activity with modifications, rather than completely stop.
While EDS and hypermobile syndromes are highly prevalent in the performing arts community, awareness of the associated complications and injury-risk factors is not fully understood with all health care providers. Seeking physical therapy treatment from a therapist that understands the physical and emotional demands of performing arts in addition to complications with EDS can make an enormous difference in an athletes career.
If you are an athlete experiencing EDS or hypermobility, and are concerned about returning to sport, give our office a call. Dr. Abbate has years of experience helping hundreds of professional performing artists at Royal Caribbean and Celebrity Cruises. If he can help them, he can help you!